Mastering Blood Sugar Safety: Your Comprehensive Guide to Staying Balanced and Healthy
Maintaining stable blood sugar levels is crucial for overall health and well-being. Whether you’re managing diabetes or simply aiming for a healthier lifestyle, understanding how blood sugar works and how to keep it in a safe range is essential. This comprehensive guide will walk you through everything you need to know about blood sugar safety, from the basics of glucose metabolism to practical tips for managing your levels effectively. Let’s dive in and empower you with the knowledge to take control of your health!

Understanding Blood Sugar Basics
Before we delve into safety measures, let’s establish a solid understanding of what blood sugar is and why it matters. Blood sugar, or glucose, is the primary source of energy for your body’s cells. It comes from the food you eat, particularly carbohydrates. When you eat carbs, your digestive system breaks them down into glucose, which then enters your bloodstream.
Why is blood sugar important? Because every cell in your body needs energy to function correctly. From powering your muscles during a workout to fueling your brain while you think, glucose is the go-to energy source.
The Role of Insulin
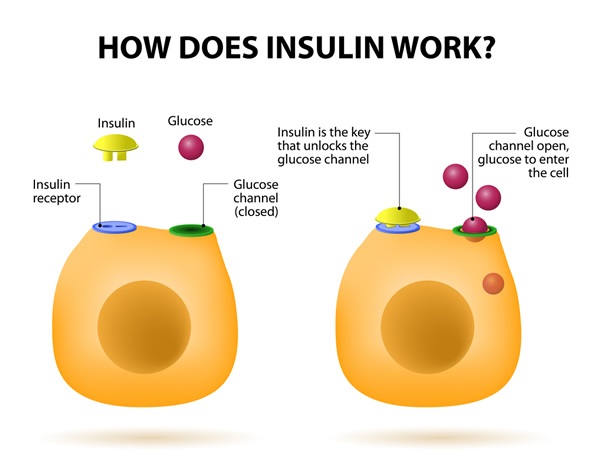
Insulin, a hormone produced by the pancreas, plays a critical role in regulating blood sugar levels. Think of insulin as a key that unlocks your cells, allowing glucose to enter and provide energy. When blood sugar levels rise after a meal, the pancreas releases insulin to help move glucose from the bloodstream into cells.
Here’s a simplified breakdown:
- You eat carbohydrates.
- Your body breaks them down into glucose.
- Glucose enters your bloodstream.
- The pancreas releases insulin.
- Insulin helps glucose move from the blood into cells.
- Fasting Blood Sugar: 70-99 mg/dL (measured after at least eight hours of fasting)
- Postprandial (After-Meal) Blood Sugar: Less than 140 mg/dL (measured two hours after starting a meal)
- Fasting Blood Sugar: 80-130 mg/dL
- Postprandial Blood Sugar: Less than 180 mg/dL
- Occurs when blood sugar levels drop too low, typically below 70 mg/dL.
- Symptoms can include shakiness, sweating, dizziness, confusion, and even loss of consciousness.
- Requires immediate treatment to raise blood sugar levels.
- Occurs when blood sugar levels are too high, typically above 180 mg/dL postprandial or 130 mg/dL fasting.
- Symptoms can include increased thirst, frequent urination, blurred vision, and fatigue.
- Requires lifestyle adjustments or medication to lower blood sugar levels.
- Wash your hands thoroughly.
- Insert a test strip into the meter.
- Prick your fingertip with a lancet.
- Apply the blood sample to the test strip.
- Wait for the meter to display your blood sugar reading.
- Accuracy: Choose a meter that is accurate and reliable. Look for models that meet international standards for accuracy.
- Ease of Use: Opt for a meter with a user-friendly interface, especially if you’re new to blood sugar monitoring.
- Features: Consider features like data storage, Bluetooth connectivity, and compatibility with continuous glucose monitoring systems.
- Continuous Monitoring: Provides a comprehensive view of blood sugar trends, rather than just snapshots at specific times.
- Alerts and Alarms: Warns you when your blood sugar is trending too high or too low.
- Data Analysis: Allows you to track your blood sugar patterns and identify factors that affect your levels.
- Type 1 Diabetes: Typically requires multiple daily checks, often before meals and at bedtime.
- Type 2 Diabetes: May require less frequent monitoring, especially if you’re managing your blood sugar with lifestyle changes alone.
- Gestational Diabetes: Often requires frequent monitoring to ensure healthy blood sugar levels during pregnancy.
- Simple Carbohydrates: Found in sugary foods, such as candy, soda, and processed snacks. They are quickly digested and can cause rapid spikes in blood sugar.
- Complex Carbohydrates: Found in whole grains, vegetables, and legumes. They are digested more slowly and provide a more sustained release of glucose into the bloodstream.
- Fiber: A type of carbohydrate that the body cannot digest. It helps slow down the absorption of glucose and can improve blood sugar control.
- Glycemic Index (GI): Measures how quickly a food raises blood sugar levels on a scale of 0 to 100. Foods with a high GI (70 or more) cause a rapid rise in blood sugar, while foods with a low GI (55 or less) have a more gradual effect.
- Glycemic Load (GL): Takes into account both the GI and the amount of carbohydrates in a serving of food. It provides a more accurate measure of a food’s impact on blood sugar levels.
- Portion Control: Be mindful of portion sizes, especially when eating carbohydrates. Overeating can lead to hyperglycemia.
- Choose Whole Foods: Opt for whole, unprocessed foods over refined and processed options. Whole foods are typically higher in fiber and nutrients and have a lower GI.
- Read Food Labels: Pay attention to the carbohydrate content and serving sizes on food labels.
- Stay Hydrated: Drink plenty of water throughout the day. Dehydration can affect blood sugar levels.
- Non-Starchy Vegetables: Broccoli, spinach, kale, bell peppers
- Lean Proteins: Chicken, fish, tofu, beans
- Healthy Fats: Avocado, nuts, seeds, olive oil
- Whole Grains: Quinoa, brown rice, oats
- Fruits: Berries, apples, pears (in moderation)
- After Exercise: Your body replenishes its glucose stores, which can also lower blood sugar levels.
- Long-Term: Regular exercise can improve insulin sensitivity and help maintain stable blood sugar levels over time.
- Choose the Right Type of Exercise: Both aerobic exercise (e.g., walking, running, swimming) and resistance training (e.g., weightlifting) can improve blood sugar control.
- Start Slowly: If you’re new to exercise, start with short, low-intensity workouts and gradually increase the duration and intensity.
- Stay Hydrated: Drink plenty of water before, during, and after exercise.
- Carry a Snack: Keep a quick-acting source of glucose, such as glucose tablets or a small juice box, with you in case your blood sugar drops too low during exercise.
- Walking: A simple and accessible form of exercise that can be easily incorporated into your daily routine.
- Swimming: A low-impact activity that is gentle on the joints.
- Cycling: A great way to improve cardiovascular health and burn calories.
- Yoga: Can help improve insulin sensitivity and reduce stress levels.
- Weightlifting: Helps build muscle mass, which can improve glucose metabolism.
- Metformin: A commonly prescribed medication that helps improve insulin sensitivity and reduce glucose production in the liver.
- Sulfonylureas: Stimulate the pancreas to release more insulin.
- DPP-4 Inhibitors: Help increase insulin production and decrease glucose production.
- SGLT2 Inhibitors: Help the kidneys remove glucose from the blood.
- GLP-1 Receptor Agonists: Increase insulin release, decrease glucose production, and slow down digestion.
- Understand the Side Effects: Be aware of the potential side effects of your medications and report any concerns to your doctor.
- Monitor Your Blood Sugar: Regularly monitor your blood sugar levels to assess how your medications are working.
- Communicate with Your Healthcare Team: Keep your doctor and other healthcare providers informed about any changes in your health or medications.
- Don’t Skip Doses: Missing doses of your medication can lead to elevated blood sugar levels.
- Shakiness
- Sweating
- Dizziness
- Confusion
- Irritability
- Hunger
- Blurred vision
- Headache
- Weakness
- Rapid heartbeat
- Loss of consciousness (in severe cases)
- Check your blood sugar: If it’s below 70 mg/dL, proceed to step 2.
- Consume 15 grams of fast-acting carbohydrates: Examples include glucose tablets, fruit juice, regular soda, or hard candy.
- Wait 15 minutes: Recheck your blood sugar after 15 minutes.
- Repeat if necessary: If your blood sugar is still below 70 mg/dL, repeat steps 2 and 3.
- Eat a meal or snack: Once your blood sugar is back in the target range, eat a meal or snack to prevent it from dropping again.
- Increased thirst
- Frequent urination
- Blurred vision
- Fatigue
- Headaches
- Slow-healing sores or cuts
- Dry, itchy skin
- Monitor Your Blood Sugar: Regularly monitor your blood sugar levels to track your progress and identify patterns.
- Adjust Your Diet: Make healthy food choices and practice portion control. Focus on complex carbohydrates, lean proteins, and healthy fats.
- Stay Active: Engage in regular physical activity to improve insulin sensitivity and lower blood sugar levels.
- Manage Stress: Stress can affect blood sugar levels. Practice stress-reducing techniques, such as meditation, yoga, or deep breathing exercises.
- Stay Hydrated: Drink plenty of water throughout the day to help flush out excess glucose.
- Get Enough Sleep: Lack of sleep can affect insulin sensitivity. Aim for 7-8 hours of quality sleep per night.
- Pack Extra Medication: Bring enough medication to last for the entire trip, plus extra in case of delays.
- Carry a Medical ID: Wear a medical ID bracelet or necklace that indicates you have diabetes.
- Pack Snacks: Bring healthy snacks to prevent hypoglycemia, especially during long flights or car rides.
- Check Your Blood Sugar Regularly: Monitor your blood sugar levels more frequently than usual, especially when adjusting to a new time zone or trying new foods.
- Stay Hydrated: Drink plenty of water to prevent dehydration.
- Be Prepared for Emergencies: Know how to access medical care in your destination.
- Be Mindful of Food Choices: Be aware of the carbohydrate content of unfamiliar foods.

What Happens When Things Go Wrong?
Problems arise when this process is disrupted. For example, in type 1 diabetes, the pancreas doesn’t produce insulin. In type 2 diabetes, the body becomes resistant to insulin, meaning the cells don’t respond properly to it. Both scenarios lead to elevated blood sugar levels, which can cause a range of health complications if left unmanaged.
Key takeaway: Keeping your blood sugar levels within a healthy range is vital for preventing these complications and maintaining optimal health.

Defining Safe Blood Sugar Levels
What exactly constitutes a “safe” blood sugar level? It varies slightly depending on individual factors such as age, overall health, and the presence of diabetes. However, general guidelines exist to help you understand where your blood sugar should ideally be.

General Blood Sugar Targets
For people without diabetes, normal blood sugar levels typically fall within the following ranges:
For individuals with diabetes, the target ranges may be slightly different, often aiming for:
It’s essential to work with your healthcare provider to determine the best target range for your specific situation. They can provide personalized recommendations based on your health history, lifestyle, and treatment plan.
Understanding Hypoglycemia and Hyperglycemia
Two primary concerns related to blood sugar safety are hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). Both conditions can be dangerous if not addressed promptly.
Hypoglycemia:
Hyperglycemia:
Being aware of the symptoms of both hypoglycemia and hyperglycemia is crucial for managing blood sugar safely. Quick recognition and appropriate action can prevent serious complications.
Monitoring Your Blood Sugar: Tools and Techniques
Regular blood sugar monitoring is a cornerstone of blood sugar safety, particularly for individuals with diabetes. Monitoring helps you understand how different factors—such as food, exercise, and medication—affect your blood sugar levels.
Blood Glucose Meters (Glucometers)
The most common tool for monitoring blood sugar is a blood glucose meter, or glucometer. These devices require a small blood sample, typically obtained by pricking your fingertip with a lancet.
How to use a glucometer:
Key Considerations:
Continuous Glucose Monitoring (CGM) Systems
Continuous glucose monitoring (CGM) systems provide real-time blood sugar readings throughout the day and night. A small sensor is inserted under the skin, typically on the abdomen or arm, and measures glucose levels in the interstitial fluid.
Benefits of CGM:
CGM systems can be particularly beneficial for individuals with type 1 diabetes or those who experience frequent episodes of hypoglycemia.
Frequency of Monitoring
How often should you monitor your blood sugar? It depends on several factors, including the type of diabetes you have, your treatment plan, and your individual needs.
Work with your healthcare provider to determine the appropriate monitoring schedule for your specific situation.
Diet and Blood Sugar: Making Smart Food Choices
What you eat has a significant impact on your blood sugar levels. Making smart food choices is crucial for maintaining stable blood sugar and preventing both hypoglycemia and hyperglycemia.
Understanding Carbohydrates
Carbohydrates are the primary nutrient that affects blood sugar levels. Different types of carbs are digested and absorbed at different rates, which can influence how quickly your blood sugar rises after eating.
Types of Carbohydrates:
Focus on choosing complex carbohydrates and high-fiber foods over simple carbohydrates to promote stable blood sugar levels.
The Glycemic Index and Glycemic Load
The glycemic index (GI) and glycemic load (GL) are tools that can help you make informed food choices.
Choosing foods with a low GI and GL can help you maintain stable blood sugar levels.
Meal Planning Tips for Blood Sugar Control
* Balance Your Meals: Include a mix of carbohydrates, protein, and healthy fats in each meal. Protein and fat help slow down the absorption of glucose and can prevent blood sugar spikes.
Examples of Blood-Sugar Friendly Foods:
By making informed food choices and practicing mindful eating, you can significantly improve your blood sugar control.
Exercise and Blood Sugar: Finding the Right Balance
Physical activity is another essential component of blood sugar safety. Exercise helps improve insulin sensitivity, which means your cells become more responsive to insulin, allowing glucose to enter and provide energy.
How Exercise Affects Blood Sugar
* During Exercise: Your muscles use glucose for energy, which can lower blood sugar levels.
However, it’s important to note that exercise can sometimes cause blood sugar levels to rise, especially during high-intensity activities. This is because the body releases stress hormones, such as adrenaline, which can temporarily increase blood sugar.
Exercise Tips for Blood Sugar Control
* Monitor Your Blood Sugar: Check your blood sugar before, during, and after exercise to understand how different activities affect your levels.
Examples of Exercises That Can Help with Blood Sugar Control:
Finding an exercise routine that you enjoy and can stick with is key to achieving long-term blood sugar control.
Medication and Blood Sugar: Working with Your Healthcare Provider
For many individuals with diabetes, medication is an essential part of managing blood sugar levels. There are various types of diabetes medications available, each with its own mechanism of action.
Types of Diabetes Medications
* Insulin: Used to replace or supplement the body’s own insulin production. It’s essential for individuals with type 1 diabetes and may be necessary for some individuals with type 2 diabetes.
It’s crucial to work closely with your healthcare provider to determine the most appropriate medication regimen for your specific needs.
Medication Safety Tips
* Follow Your Doctor’s Instructions: Take your medications exactly as prescribed.
Remember, medication is just one piece of the puzzle. Lifestyle changes, such as diet and exercise, are also essential for managing blood sugar effectively.
Managing Hypoglycemia: Quick Action Steps
Hypoglycemia, or low blood sugar, can occur suddenly and requires prompt treatment. Knowing how to recognize and manage hypoglycemia is crucial for blood sugar safety.
Recognizing Hypoglycemia
Symptoms of hypoglycemia can vary from person to person, but common signs include:
If you experience any of these symptoms, check your blood sugar immediately.
Treating Hypoglycemia
The “15-15 Rule” is a simple and effective way to treat mild to moderate hypoglycemia:
For severe hypoglycemia (loss of consciousness), glucagon may be needed. Glucagon is a hormone that raises blood sugar levels. It’s typically administered by injection or nasal spray. Family members or caregivers should be trained on how to administer glucagon in case of an emergency.
Key Takeaway: Always carry a source of fast-acting carbohydrates with you and ensure that your family and friends know how to recognize and treat hypoglycemia.
Managing Hyperglycemia: Long-Term Strategies
Hyperglycemia, or high blood sugar, can also lead to serious health complications if left unmanaged. While occasional spikes in blood sugar are normal, consistently high levels require attention and long-term strategies.
Identifying Hyperglycemia
Symptoms of hyperglycemia can develop gradually over time. Common signs include:
If you experience these symptoms, check your blood sugar regularly and consult with your healthcare provider.
Strategies for Managing Hyperglycemia
* Follow Your Treatment Plan: Adhere to your prescribed medication regimen and lifestyle recommendations.
If your blood sugar levels are consistently high despite your best efforts, consult with your healthcare provider. They may need to adjust your medication or treatment plan.
Blood Sugar Safety During Travel
Traveling can disrupt your normal routine and make it challenging to manage your blood sugar levels. Planning ahead and taking extra precautions can help you stay safe and healthy while on the go.
Pre-Travel Checklist
* Consult with Your Healthcare Provider: Discuss your travel plans with your doctor and get any necessary prescriptions or recommendations.
Tips for Managing Blood Sugar While Traveling
* Adjust Insulin Doses: If you’re traveling across time zones, you may need to adjust your insulin doses. Consult with your doctor for guidance.
Leave a Reply