Navigating Blood Sugar Safety: Your Comprehensive Guide to Staying Balanced and Healthy
Maintaining stable blood sugar levels is crucial for overall health and well-being. Think of your blood sugar as the fuel gauge for your body – too high or too low, and things can start to sputter. This comprehensive guide will walk you through understanding blood sugar, recognizing potential dangers, and implementing practical strategies to keep your levels in a safe and healthy range. Whether you’re managing diabetes or simply aiming for a healthier lifestyle, this information will empower you to take control of your blood sugar safety.

Understanding Blood Sugar: The Basics
Blood sugar, also known as glucose, is the primary source of energy for your body. It comes from the food you eat, and your body uses insulin, a hormone produced by the pancreas, to help glucose enter your cells for energy. Understanding how this process works is the first step in maintaining blood sugar safety.

What is Normal Blood Sugar?
Normal blood sugar levels vary depending on when you check them. Here’s a general guideline:
- Fasting Blood Sugar: 70-99 mg/dL (milligrams per deciliter)
- 2 Hours After Eating: Less than 140 mg/dL
- Food: The type and amount of carbohydrates you consume have the most significant impact.
- Physical Activity: Exercise can lower blood sugar as your muscles use glucose for energy.
- Stress: Stress hormones can raise blood sugar levels.
- Illness: Being sick can also cause blood sugar fluctuations.
- Medications: Certain medications, like steroids, can affect blood sugar.
- Sleep: Lack of sleep can impact insulin sensitivity.
- Increased thirst
- Frequent urination
- Blurred vision
- Fatigue
- Headaches
- Cardiovascular Disease: High blood sugar can damage blood vessels, increasing the risk of heart attack and stroke.
- Nerve Damage (Neuropathy): This can cause numbness, tingling, and pain, especially in the hands and feet.
- Kidney Damage (Nephropathy): High blood sugar can impair kidney function, potentially leading to kidney failure.
- Eye Damage (Retinopathy): This can lead to vision loss and blindness.
- Foot Problems: Nerve damage and poor circulation can increase the risk of foot ulcers and infections.
- Shakiness
- Sweating
- Dizziness
- Confusion
- Irritability
- Hunger
- Rapid heartbeat
- Blurred vision
- Seizures (in severe cases)
- Loss of consciousness (in severe cases)
- Skipping meals
- Taking too much insulin or diabetes medication
- Excessive exercise without adequate carbohydrate intake
- Drinking alcohol, especially on an empty stomach
- Consume 15 grams of fast-acting carbohydrates (e.g., glucose tablets, juice, regular soda).
- Wait 15 minutes and check your blood sugar again.
- If your blood sugar is still below 70 mg/dL, repeat steps 1 and 2.
- Once your blood sugar is above 70 mg/dL, eat a snack or meal to prevent it from dropping again.
- Focus on Complex Carbohydrates: Choose whole grains, vegetables, and fruits over refined grains and sugary snacks. These foods are digested more slowly, leading to a more gradual rise in blood sugar.
- Example: Opt for brown rice instead of white rice, or choose whole-wheat bread over white bread.
- Control Portion Sizes: Overeating can lead to a spike in blood sugar. Use smaller plates and measure your portions to avoid overconsumption.
- Limit Sugary Drinks and Processed Foods: These items are often high in sugar and low in nutrients, causing rapid blood sugar spikes.
- Include Protein and Healthy Fats: Adding protein and healthy fats to your meals can help slow down the absorption of carbohydrates and promote stable blood sugar levels.
- Examples: Include lean meats, poultry, fish, beans, nuts, and avocados in your diet.
- Eat Regularly: Skipping meals can lead to both high and low blood sugar levels. Aim for consistent meal times and avoid long gaps between eating.
- Consider the Glycemic Index (GI): The GI measures how quickly a food raises blood sugar levels. Choosing foods with a low GI can help maintain more stable levels.
- Examples of Low GI Foods: Most fruits and vegetables, whole grains, legumes, nuts.
- Examples of High GI Foods: White bread, sugary drinks, processed snacks.
- Aim for Regular Exercise: The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic exercise per week, spread out over at least three days.
- Choose Activities You Enjoy: Whether it’s walking, swimming, cycling, or dancing, find activities you find enjoyable to make exercise a sustainable part of your routine.
- Monitor Blood Sugar Before, During, and After Exercise: This will help you understand how your body responds to different types of exercise and adjust your food intake or medication accordingly.
- Stay Hydrated: Drink plenty of water before, during, and after exercise to prevent dehydration and maintain optimal blood sugar levels.
- Incorporate Strength Training: Strength training can help build muscle mass, which improves insulin sensitivity and helps regulate blood sugar.
- Practice Relaxation Techniques: Deep breathing exercises, meditation, and yoga can help reduce stress and lower blood sugar levels.
- Get Enough Sleep: Lack of sleep can increase stress hormones and impair insulin sensitivity. Aim for 7-8 hours of quality sleep per night.
- Engage in Hobbies: Spending time doing things you enjoy can help reduce stress and improve your overall well-being.
- Seek Support: Talking to a therapist, counselor, or support group can provide valuable tools for managing stress.
- Limit Caffeine and Alcohol: These substances can exacerbate stress and negatively impact blood sugar levels.
- Take Medications as Prescribed: Follow your doctor’s instructions carefully and don’t skip doses.
- Monitor Blood Sugar Regularly: Regular blood sugar monitoring is essential for understanding how your medications are working and making adjustments as needed.
- Communicate with Your Doctor: Keep your doctor informed about any changes in your health, lifestyle, or medications.
- Understand the Side Effects: Be aware of the potential side effects of your medications and report any concerns to your doctor.
- Carry Identification: Wear a medical ID bracelet or necklace that indicates you have diabetes and lists any medications you’re taking.
- Use a Blood Glucose Meter: Follow the instructions provided with your meter and test your blood sugar at the times recommended by your doctor.
- Keep a Log: Record your blood sugar readings, along with any relevant information, such as food intake, exercise, and medications.
- Continuous Glucose Monitoring (CGM): Consider using a CGM, which continuously tracks your blood sugar levels and provides real-time data.
- Work with Your Healthcare Team: Share your blood sugar logs with your doctor or diabetes educator to help them adjust your treatment plan as needed.
- Drink Plenty of Water: Water helps to dilute the glucose in your bloodstream and allows your kidneys to flush out excess sugar through urine.
- Avoid Sugary Drinks: Opt for water instead of sugary sodas, juices, and sweetened beverages, which can cause rapid spikes in blood sugar.
- Monitor Urine Color: Pale yellow urine is a good indicator of adequate hydration. Darker urine may indicate dehydration.
- Drink Throughout the Day: Don’t wait until you’re thirsty to drink. Sip on water consistently throughout the day to maintain optimal hydration levels.
- Consider Electrolyte Balance: If you’re exercising or sweating heavily, consider replenishing electrolytes with a sports drink or electrolyte-rich foods.
- Identify Your Target Blood Sugar Range: Work with your doctor to determine your ideal blood sugar range, both before and after meals.
- Develop a Meal Plan: Work with a registered dietitian or diabetes educator to create a meal plan that meets your nutritional needs and helps you maintain stable blood sugar levels.
- Establish an Exercise Routine: Incorporate regular physical activity into your daily routine, and monitor your blood sugar levels before, during, and after exercise.
- Create a Stress Management Plan: Identify your stressors and develop strategies for managing them effectively.
- Know How to Treat Hypoglycemia and Hyperglycemia: Be prepared to recognize and treat both high and low blood sugar levels.
- Carry Emergency Supplies: Always carry a source of fast-acting carbohydrates (e.g., glucose tablets) in case of hypoglycemia.
- Educate Your Family and Friends: Make sure your loved ones know how to recognize and treat hypoglycemia, and that they know where to find your emergency supplies.
- Review and Update Your Plan Regularly: Your blood sugar safety plan should be reviewed and updated regularly to ensure that it continues to meet your needs.
- Pack Extra Medication and Supplies: Always pack extra medication and supplies in case of delays or unexpected events.
- Carry a Medical ID: Wear a medical ID bracelet or necklace that indicates you have diabetes and lists any medications you’re taking.
- Plan Your Meals: Research restaurants and grocery stores in advance to ensure that you have access to healthy food options.
- Adjust Insulin Doses as Needed: If you’re changing time zones, work with your doctor to adjust your insulin doses accordingly.
- Monitor Blood Sugar More Frequently: Check your blood sugar more frequently than usual to ensure that it stays within your target range.
- Stay Hydrated: Drink plenty of water to prevent dehydration.
- Be Prepared for Emergencies: Know how to treat hypoglycemia and hyperglycemia, and carry a source of fast-acting carbohydrates with you at all times.
These are general targets, and your doctor may recommend slightly different ranges based on your individual health profile.
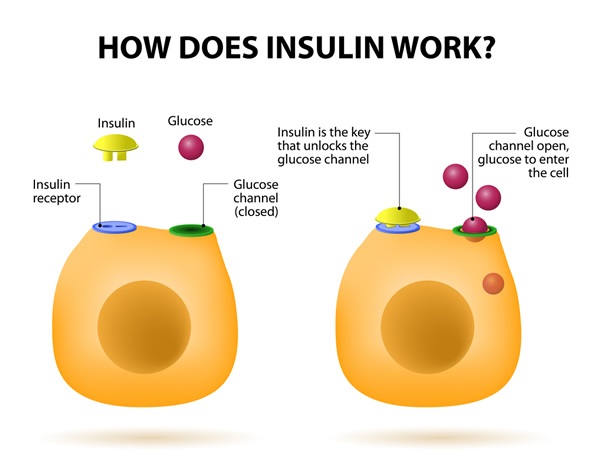
The Role of Insulin
Insulin acts like a key, unlocking your cells to allow glucose to enter and be used for energy. When you eat, your blood sugar rises, signaling the pancreas to release insulin. This helps to lower blood sugar back to a normal level. Problems arise when the body doesn’t produce enough insulin (as in type 1 diabetes) or when the body becomes resistant to insulin’s effects (as in type 2 diabetes).

Factors Affecting Blood Sugar Levels
Many factors can influence your blood sugar levels, including:
Understanding these factors can help you better anticipate and manage your blood sugar levels.

Recognizing the Dangers: High and Low Blood Sugar
Both high and low blood sugar levels can pose significant health risks. Recognizing the symptoms and understanding the potential complications is essential for maintaining blood sugar safety.
Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when there’s too much glucose in the blood. Over time, consistently high blood sugar can lead to serious complications.
Symptoms of Hyperglycemia:
Long-Term Complications of Hyperglycemia:
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop too low. This can happen quickly and requires immediate attention.
Symptoms of Hypoglycemia:
Causes of Hypoglycemia:
Treating Hypoglycemia:
If you experience symptoms of hypoglycemia, it’s crucial to act quickly. Follow the “15-15 rule”:
Important Note: If someone is unconscious or unable to swallow, do not attempt to give them food or drink. Administer glucagon (if available) and call for emergency medical assistance immediately.
Strategies for Maintaining Blood Sugar Safety
Now that you understand the risks of high and low blood sugar, let’s explore practical strategies for maintaining stable and healthy levels.
Dietary Management
What you eat has a direct impact on your blood sugar. Making informed food choices is a cornerstone of blood sugar safety.
The Power of Physical Activity
Regular physical activity is a powerful tool for managing blood sugar. It helps your body use insulin more effectively and can lower blood sugar levels.
Stress Management Techniques
Stress can significantly impact blood sugar levels. When you’re stressed, your body releases hormones that can raise blood sugar. Managing stress effectively is crucial for blood sugar safety.
Medication Management
If you have diabetes, medication is often a necessary part of managing your blood sugar. It’s crucial to take your medications as prescribed and to understand how they work.
Regular Blood Sugar Monitoring
Regular blood sugar monitoring is the cornerstone of blood sugar safety, especially for individuals with diabetes. It provides valuable insights into how your body responds to food, exercise, stress, and medication.
The Importance of Hydration
Staying properly hydrated is essential for overall health and plays a significant role in blood sugar management. Dehydration can lead to higher blood sugar concentrations, making it harder for your body to regulate levels effectively.
Creating a Blood Sugar Safety Plan
Developing a personalized blood sugar safety plan is essential for effectively managing your blood sugar levels and preventing dangerous fluctuations. This plan should be tailored to your individual needs and circumstances, and it should be developed in consultation with your healthcare team.
Blood Sugar Safety While Traveling
Traveling can disrupt your normal routine and make it more challenging to manage your blood sugar. Planning ahead and taking precautions can help you stay safe and healthy while on the go.
Conclusion: Empowering Yourself for Blood Sugar Safety
Maintaining blood sugar safety is an ongoing journey that requires knowledge, vigilance, and a proactive approach. By understanding the basics of blood sugar, recognizing the dangers of high and low levels, and implementing practical strategies for management, you can empower yourself to live a healthier and more balanced life. Remember to work closely with your healthcare team to develop a personalized plan that meets your individual needs and goals. Staying informed, staying consistent, and staying proactive will help you navigate the path to blood sugar safety with confidence.
Key Takeaway: Consistent monitoring, a balanced diet, regular exercise, and effective stress management are the cornerstones of blood sugar safety.
Internal Link Suggestion: For more information on healthy eating habits, read our article on “The Ultimate Guide to Balanced Nutrition.”
External Link Suggestion: For more information on diabetes management, visit the American Diabetes Association website: “American Diabetes Association.”
Leave a Reply