Navigating Blood Sugar Safety: Your Friendly Guide to Staying Balanced
Maintaining stable blood sugar levels is essential for overall health and well-being. Whether you’re managing diabetes or simply aiming for a healthier lifestyle, understanding blood sugar safety is key. This guide provides a friendly, comprehensive overview of what you need to know to keep your blood sugar balanced and stay healthy.

Understanding Blood Sugar: The Basics
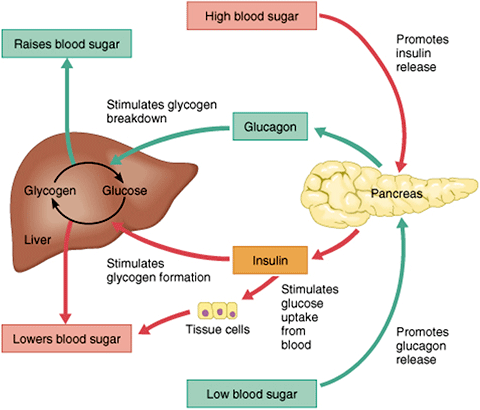
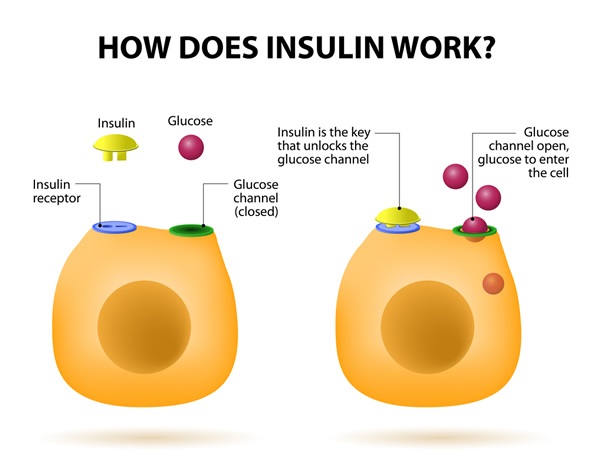
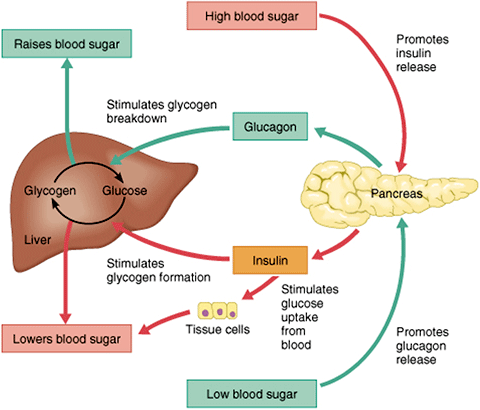
Blood sugar, or glucose, is the primary source of energy for your body. It comes from the food you eat and is carried to your cells by the bloodstream. Insulin, a hormone produced by the pancreas, helps glucose enter your cells to be used for energy. When this process works smoothly, your blood sugar levels remain within a healthy range. But what happens when things go awry?

What is Blood Sugar and Why Does It Matter?
Blood sugar levels fluctuate throughout the day, depending on when you eat, how much you eat, and your activity level. Maintaining stable blood sugar is crucial because consistently high or low levels can lead to serious health complications.
Here’s why it matters:
- Energy Levels: Stable blood sugar provides a consistent energy supply, preventing energy crashes and fatigue.
- Organ Function: Balanced blood sugar supports the proper functioning of vital organs like the brain, heart, and kidneys.
- Disease Prevention: Keeping blood sugar in check reduces the risk of developing type 2 diabetes, heart disease, and nerve damage.
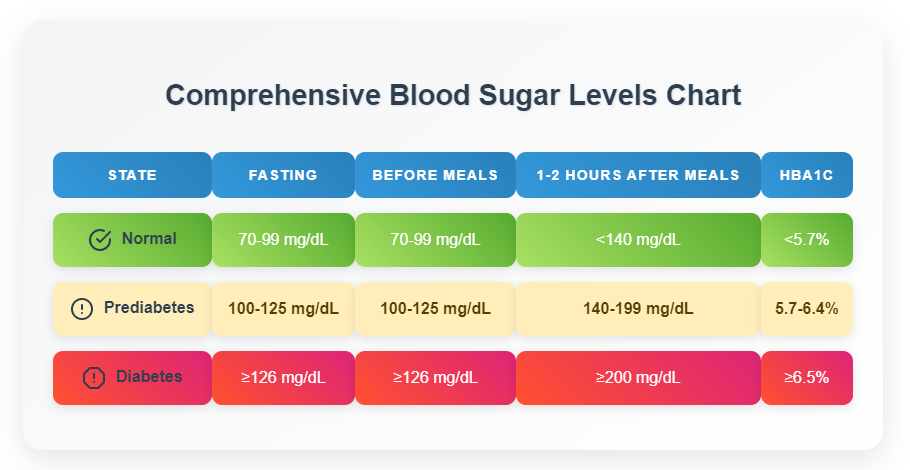
- Fasting Blood Sugar (after at least 8 hours of not eating): 70-99 mg/dL
- Two Hours After Eating: Less than 140 mg/dL
- A1C (average blood sugar over 2-3 months): Less than 5.7%
- Dietary Choices: Eating too many carbohydrates or sugary foods.
- Lack of Exercise: Physical inactivity reduces the body’s ability to use glucose for energy.
- Insufficient Insulin: In individuals with diabetes, not taking enough insulin or oral medication.
- Illness or Stress: These can cause hormonal changes that affect blood sugar levels.
- Increased Thirst: The body tries to flush out excess glucose through urination, leading to dehydration and increased thirst.
- Frequent Urination: High blood sugar levels overwhelm the kidneys, causing them to produce more urine.
- Blurred Vision: High glucose levels can affect the lens of the eye, leading to temporary vision changes.
- Fatigue: Despite having plenty of glucose in the blood, cells can’t access it effectively, resulting in fatigue.
- Headaches: Fluctuations in blood sugar can trigger headaches.
- Excess Insulin: Taking too much insulin or certain diabetes medications.
- Skipping Meals: Not eating enough food, especially after taking insulin or medication.
- Intense Exercise: Strenuous physical activity can deplete glucose stores.
- Alcohol Consumption: Alcohol can interfere with the liver’s ability to release glucose.
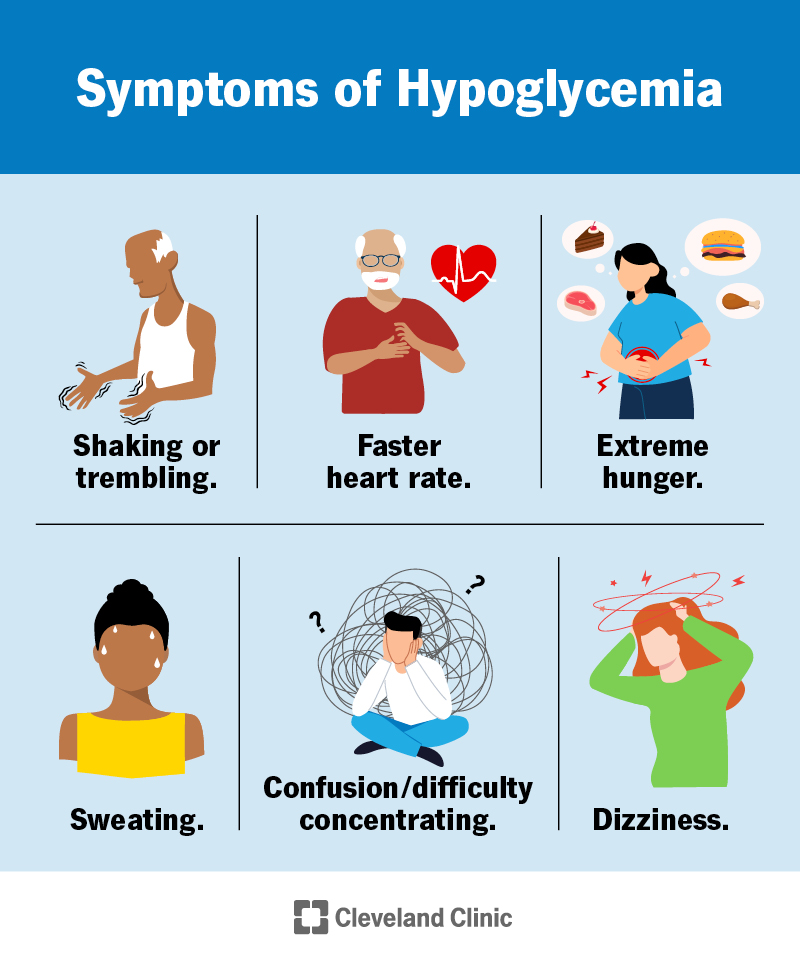
- Shakiness: Low blood sugar can cause tremors and shakiness.
- Sweating: The body releases adrenaline in response to low blood sugar, leading to sweating.
- Dizziness: Insufficient glucose in the brain can cause dizziness and lightheadedness.
- Confusion: Low blood sugar can impair cognitive function, leading to confusion and difficulty concentrating.
- Irritability: Blood sugar fluctuations can affect mood, causing irritability and anxiety.
- Rapid Heartbeat: The body tries to compensate for low blood sugar by increasing heart rate.
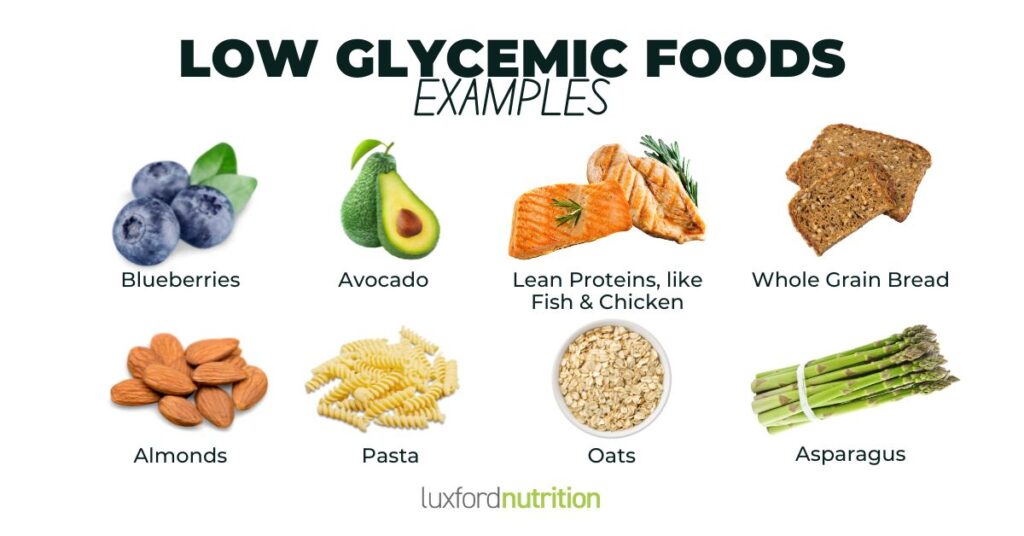
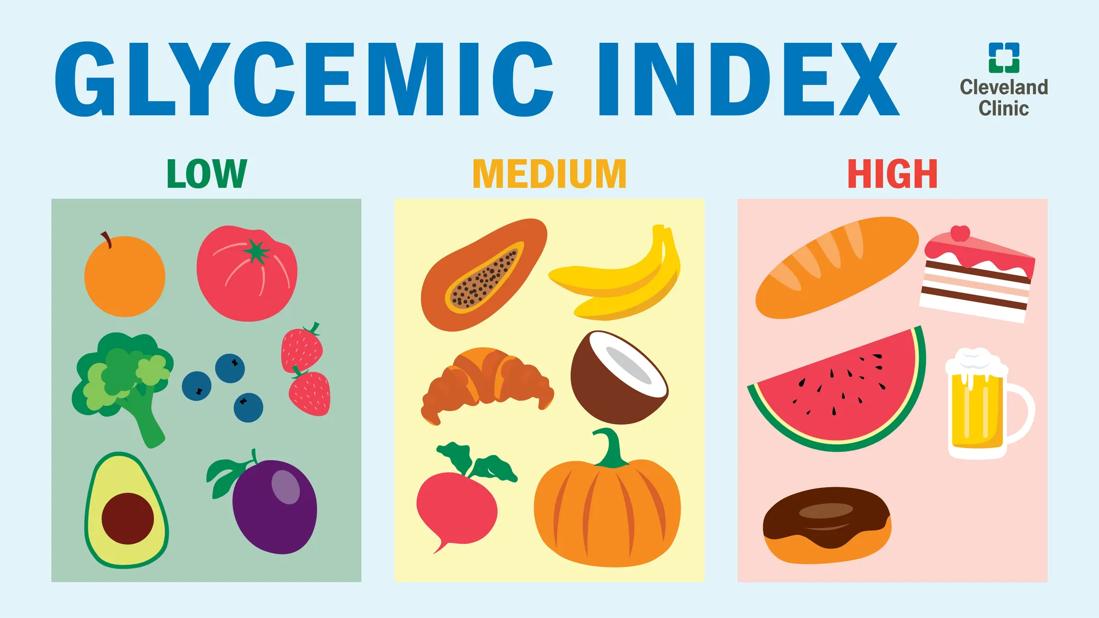
- Choose Low-Glycemic Index (GI) Foods: The glycemic index measures how quickly a food raises blood sugar levels. Opt for low-GI foods like whole grains, non-starchy vegetables, and legumes.
- Balance Your Meals: Include a mix of carbohydrates, protein, and healthy fats in each meal to slow down glucose absorption.
- Portion Control: Eating smaller, more frequent meals can help prevent blood sugar spikes.
- Limit Sugary Drinks and Processed Foods: These can cause rapid increases in blood sugar levels.
- Increase Fiber Intake: Fiber slows down the absorption of glucose, helping to stabilize blood sugar levels. Good sources of fiber include fruits, vegetables, and whole grains.
- Breakfast: Oatmeal with berries and nuts
- Lunch: Salad with grilled chicken or tofu and a variety of non-starchy vegetables
- Dinner: Baked salmon with roasted vegetables and quinoa
- Snacks: Apple slices with almond butter, Greek yogurt with berries, or a handful of nuts
- Aerobic Exercise: Activities like walking, jogging, swimming, and cycling can help lower blood sugar levels and improve cardiovascular health.
- Strength Training: Building muscle mass can improve insulin sensitivity and help regulate blood sugar levels.
- Consistency is Key: Aim for at least 150 minutes of moderate-intensity exercise per week, spread out over several days.
- Check Blood Sugar Before and After Exercise: Monitor your blood sugar levels to understand how different types of exercise affect you.
- Stay Hydrated: Drink plenty of water to prevent dehydration, which can affect blood sugar levels.
- Carry a Snack: Keep a fast-acting source of glucose on hand in case your blood sugar drops too low during exercise.
- Blood Glucose Meter: This is the most common tool for checking blood sugar levels. It involves pricking your finger with a lancet and placing a drop of blood on a test strip, which is then inserted into the meter.
- Continuous Glucose Monitor (CGM): A CGM is a small device that’s inserted under the skin and continuously monitors glucose levels throughout the day and night. It provides real-time data and alerts you when your blood sugar is too high or too low.
- Follow Your Healthcare Provider’s Recommendations: They can help you determine how often you should check your blood sugar and what your target ranges should be.
- Keep a Log: Record your blood sugar readings, along with information about your meals, activities, and medications. This can help you identify patterns and make informed decisions about your diabetes management plan.
- Calibrate Your Meter Regularly: Ensure your blood glucose meter is accurate by calibrating it according to the manufacturer’s instructions.
- Insulin: Insulin is a hormone that helps glucose enter your cells. It’s available in various forms, including rapid-acting, short-acting, intermediate-acting, and long-acting.
- Oral Medications: Several types of oral medications can help lower blood sugar levels, including metformin, sulfonylureas, and DPP-4 inhibitors.
- Follow Your Healthcare Provider’s Instructions: Take your medications exactly as prescribed and don’t change the dosage without consulting your doctor.
- Understand Potential Side Effects: Be aware of the potential side effects of your medications and report any concerns to your healthcare provider.
- Monitor Blood Sugar Regularly: Regularly check your blood sugar levels to assess how well your medications are working.
- Identify Your Stressors: Determine what triggers your stress and develop strategies for managing them.
- Practice Relaxation Techniques: Techniques like deep breathing, meditation, and yoga can help reduce stress and lower blood sugar levels.
- Get Enough Sleep: Lack of sleep can increase stress hormones and affect blood sugar control. Aim for 7-8 hours of sleep per night.
- Engage in Hobbies: Make time for activities you enjoy, such as reading, gardening, or spending time with loved ones.
- Drink in Moderation: If you choose to drink alcohol, do so in moderation. For women, this means no more than one drink per day, and for men, no more than two drinks per day.
- Eat While Drinking: Always eat something when you drink alcohol to help stabilize your blood sugar levels.
- Monitor Your Blood Sugar: Check your blood sugar levels before, during, and after drinking alcohol.
- Be Aware of Hypoglycemia: Alcohol can interfere with the liver’s ability to release glucose, increasing the risk of hypoglycemia.
- High Blood Sugar Levels: Typically above 300 mg/dL
- Ketones in Urine: Ketones are produced when the body breaks down fat for energy due to a lack of insulin.
- Fruity-Scented Breath: This is caused by the presence of ketones.
- Nausea and Vomiting: High ketone levels can cause nausea and vomiting.
- Abdominal Pain: DKA can cause severe abdominal pain.
- Rapid, Deep Breathing: The body tries to get rid of excess carbon dioxide.
- Check Blood Sugar and Ketone Levels: Use a blood glucose meter and ketone test strips to confirm the diagnosis.
- Administer Insulin: Follow your healthcare provider’s instructions for administering insulin.
- Stay Hydrated: Drink plenty of water to help flush out excess glucose and ketones.
- Seek Medical Attention: If you suspect DKA, seek immediate medical attention.
- Loss of Consciousness: The individual is unresponsive and unable to follow commands.
- Seizures: Uncontrolled muscle contractions.
- Administer Glucagon: If the individual is unconscious or unable to swallow, administer glucagon, a hormone that raises blood sugar levels.
- Call for Help: Call emergency services immediately.
- Provide Glucose: Once the individual regains consciousness, give them a fast-acting source of glucose, such as juice or glucose tablets.
- Maintain Healthy Blood Sugar Levels: Keep your blood sugar within the target range recommended by your healthcare provider.
- Manage Blood Pressure and Cholesterol: High blood pressure and cholesterol can further increase the risk of cardiovascular disease.
- Quit Smoking: Smoking damages blood vessels and increases the risk of heart disease.
- Maintain Healthy Blood Sugar Levels: Keep your blood sugar within the target range recommended by your healthcare provider.
- Regular Foot Care: Inspect your feet daily for cuts, blisters, and other signs of injury.
- Proper Footwear: Wear comfortable shoes that fit well.
- Maintain Healthy Blood Sugar Levels: Keep your blood sugar within the target range recommended by your healthcare provider.
- Manage Blood Pressure: High blood pressure can further damage the kidneys.
- Regular Kidney Function Tests: Get regular kidney function tests to monitor your kidney health.
- Maintain Healthy Blood Sugar Levels: Keep your blood sugar within the target range recommended by your healthcare provider.
- Regular Eye Exams: Get regular eye exams to detect and treat retinopathy early.
- Regular Monitoring: Monitor blood sugar levels regularly.
- Dietary Changes: Follow a healthy diet that’s low in sugar and processed foods.
- Exercise: Engage in regular physical activity.
- Medication: Some women may need insulin or oral medications to manage their blood sugar levels.
- Insulin Therapy: Administer insulin as prescribed by the healthcare provider.
- Blood Sugar Monitoring: Monitor blood sugar levels regularly.
- Dietary Management: Follow a healthy diet that’s low in sugar and processed foods.
- Education: Educate children and their caregivers about diabetes management.
- Simplified Treatment Plans: Develop simplified treatment plans that are easy to follow.
- Medication Management: Review medications regularly to avoid drug interactions.
- Fall Prevention: Take steps to prevent falls, which can be more serious for seniors with diabetes.
- Social Support: Encourage social interaction and support to prevent isolation and depression.
- Anchor Text: “normal blood sugar ranges” – Link to the section “Normal Blood Sugar Ranges: A Quick Reference” within this article.
- Anchor Text: “dietary strategies” – Link to the section “Dietary Strategies for Blood Sugar Control” within this article.
- Anchor Text: “exercise in blood sugar management” – Link to the section “The Role of Exercise in Blood Sugar Management” within this article.
- Anchor Text: “continuous glucose monitor” – Link to the section “Monitoring Your Blood Sugar: Tools and Techniques” within this article.
- Anchor Text: “symptoms of hypoglycemia” – Link to the section “Hypoglycemia (Low Blood Sugar): Symptoms and Causes” within this article.
- American Diabetes Association: https://www.diabetes.org/ (Link with anchor text: “American Diabetes Association” – opens in a new tab, rel=”noopener nofollow”)
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): https://www.niddk.nih.gov/ (Link with anchor text: “NIDDK” – opens in a new tab, rel=”noopener nofollow”)
- Mayo Clinic – Diabetes: [https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371

Normal Blood Sugar Ranges: A Quick Reference
Understanding normal blood sugar ranges is the first step in blood sugar safety. These ranges can vary slightly depending on individual circumstances and testing methods, but here’s a general guideline:
If your blood sugar levels consistently fall outside these ranges, it’s important to consult with a healthcare provider.

Recognizing High and Low Blood Sugar
Being able to recognize the symptoms of high and low blood sugar is crucial for taking timely action and preventing complications.
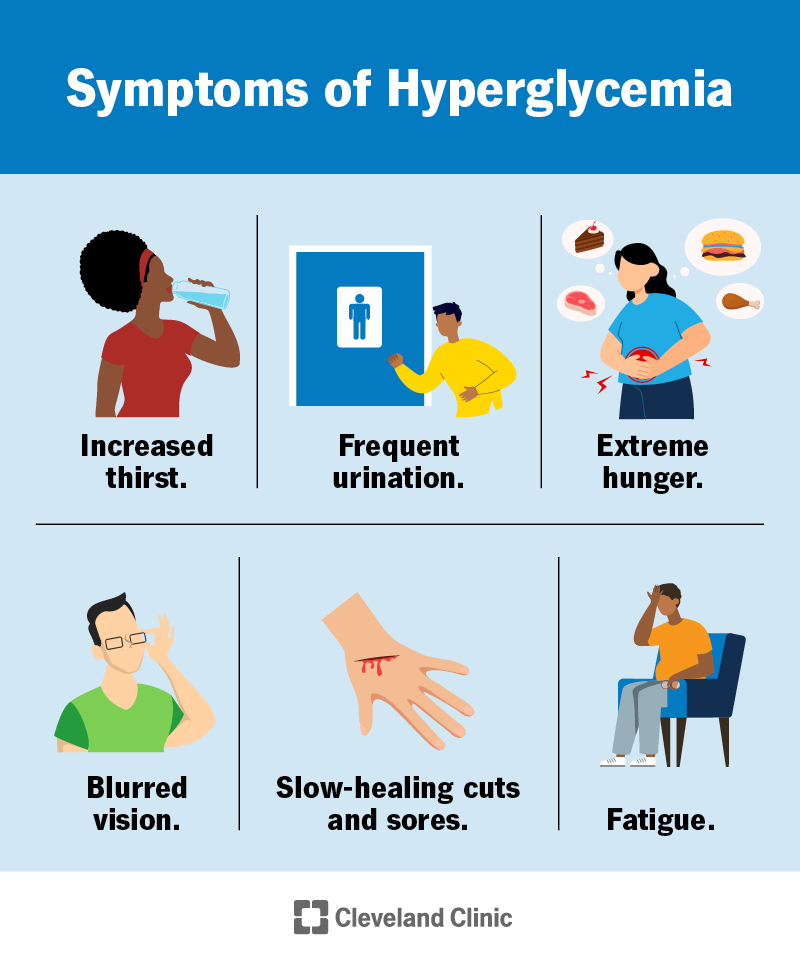
Hyperglycemia (High Blood Sugar): Symptoms and Causes
Hyperglycemia occurs when there’s too much glucose in the blood. This can happen for various reasons, including:
Symptoms of Hyperglycemia:
If you experience these symptoms, it’s important to check your blood sugar levels and take appropriate action, such as adjusting your diet, exercise, or medication as directed by your healthcare provider.
Hypoglycemia (Low Blood Sugar): Symptoms and Causes
Hypoglycemia occurs when there’s not enough glucose in the blood. This can happen due to:
Symptoms of Hypoglycemia:
If you experience these symptoms, it’s important to check your blood sugar levels immediately. If your blood sugar is low (typically below 70 mg/dL), consume a fast-acting source of glucose, such as glucose tablets, juice, or hard candy. Recheck your blood sugar after 15 minutes, and repeat if necessary.
Practical Tips for Maintaining Blood Sugar Safety
Now that you understand the basics of blood sugar and how to recognize high and low levels, let’s dive into practical tips for maintaining blood sugar safety.
Dietary Strategies for Blood Sugar Control
What you eat has a significant impact on your blood sugar levels. Here are some dietary strategies to help you maintain stable blood sugar:
Example Meal Plan for Blood Sugar Control:
The Role of Exercise in Blood Sugar Management
Regular physical activity is essential for blood sugar management. Exercise helps improve insulin sensitivity, which means your body can use insulin more effectively to lower blood sugar levels.
Important Considerations:
Monitoring Your Blood Sugar: Tools and Techniques
Regularly monitoring your blood sugar levels is crucial for understanding how your body responds to different foods, activities, and medications.
Tips for Effective Blood Sugar Monitoring:
Medication Management: Insulin and Other Drugs
For many individuals with diabetes, medication is an essential part of blood sugar management.
Important Considerations:
Stress Management and Its Impact on Blood Sugar
Stress can have a significant impact on blood sugar levels. When you’re stressed, your body releases hormones like cortisol and adrenaline, which can raise blood sugar levels.
Alcohol and Blood Sugar: What You Need to Know
Alcohol can affect blood sugar levels in complex ways. It can initially lower blood sugar, but it can also lead to hyperglycemia later on.
Emergency Situations: What to Do When Blood Sugar Levels Are Dangerously High or Low
Despite your best efforts, there may be times when your blood sugar levels become dangerously high or low. Knowing how to respond in these situations is crucial.
Managing Severe Hyperglycemia
Severe hyperglycemia can lead to a condition called diabetic ketoacidosis (DKA), which is a life-threatening emergency.
Symptoms of DKA:
What to Do:
Managing Severe Hypoglycemia
Severe hypoglycemia can lead to seizures, loss of consciousness, and even death.
Symptoms of Severe Hypoglycemia:
What to Do:
Long-Term Complications of Uncontrolled Blood Sugar
Uncontrolled blood sugar can lead to a variety of long-term complications that affect various parts of the body.
Cardiovascular Disease
High blood sugar levels can damage blood vessels, increasing the risk of heart disease, stroke, and peripheral artery disease.
Prevention:
Nerve Damage (Neuropathy)
High blood sugar levels can damage nerves, leading to neuropathy. This can cause pain, numbness, and tingling in the hands and feet.
Prevention:
Kidney Damage (Nephropathy)
High blood sugar levels can damage the kidneys, leading to nephropathy. This can eventually lead to kidney failure.
Prevention:
Eye Damage (Retinopathy)
High blood sugar levels can damage the blood vessels in the retina, leading to retinopathy. This can cause vision loss and blindness.
Prevention:
Blood Sugar Safety in Specific Populations
Blood sugar safety is particularly important for certain populations, including pregnant women, children, and seniors.
Pregnancy and Gestational Diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. It can increase the risk of complications for both the mother and the baby.
Management:
Children and Type 1 Diabetes
Type 1 diabetes is an autoimmune condition that usually develops in childhood. It requires lifelong insulin therapy.
Management:
Seniors and Diabetes
Seniors with diabetes may face unique challenges, such as cognitive impairment, mobility issues, and polypharmacy.
Management:
Conclusion: Taking Control of Your Blood Sugar Health
Maintaining blood sugar safety is a lifelong journey that requires knowledge, commitment, and support. By understanding the basics of blood sugar, recognizing the symptoms of high and low blood sugar, and implementing practical strategies for blood sugar control, you can take control of your health and prevent serious complications. Remember to work closely with your healthcare provider to develop a personalized plan that meets your individual needs. Your health is your wealth, and taking proactive steps to manage your blood sugar is an investment in a healthier, happier future.
Internal Linking Suggestions:
External Linking Suggestions: