Navigating Blood Sugar Safety: Your Comprehensive Guide to Staying Balanced
Maintaining stable blood sugar levels is crucial for overall health and well-being. Whether you’re managing diabetes, pre-diabetes, or simply aiming for a healthier lifestyle, understanding blood sugar safety is essential. This guide will provide you with a comprehensive overview of blood sugar, including how it works, potential dangers, and practical tips to keep it within a healthy range. Let’s embark on this journey together and empower ourselves with the knowledge needed to thrive!

Understanding Blood Sugar Basics
Blood sugar, or glucose, is the primary source of energy for our bodies. It comes from the food we eat, primarily carbohydrates. When we consume carbohydrates, our digestive system breaks them down into glucose, which then enters the bloodstream. From there, insulin, a hormone produced by the pancreas, helps glucose move from the blood into our cells, where it’s used for energy.
Think of insulin as the key that unlocks the door to your cells, allowing glucose to enter and provide fuel. When this process works smoothly, our blood sugar levels remain within a healthy range. However, when there’s a problem with insulin production or function, blood sugar levels can become imbalanced, leading to various health issues.
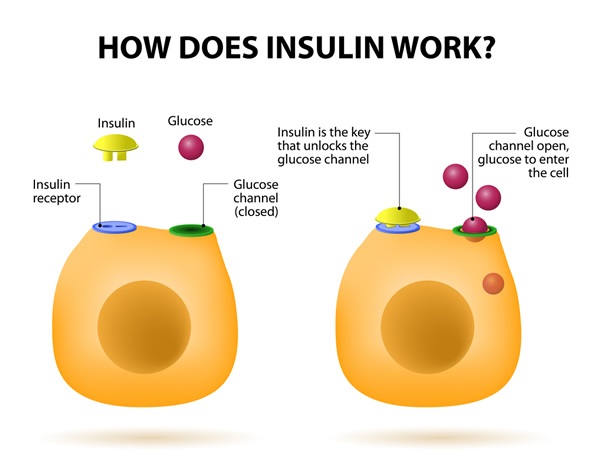
The Role of Insulin
Insulin plays a pivotal role in regulating blood sugar levels. After a meal, as glucose levels rise, the pancreas releases insulin to facilitate glucose uptake by cells. This process helps lower blood sugar back to a normal level. Without sufficient insulin or when cells become resistant to insulin’s effects, glucose accumulates in the bloodstream, leading to hyperglycemia (high blood sugar).

Normal Blood Sugar Ranges
Understanding normal blood sugar ranges is the first step in maintaining blood sugar safety. These ranges can vary slightly depending on individual factors and the specific guidelines used by healthcare providers. However, generally accepted ranges include:
- Fasting Blood Sugar: 70-99 mg/dL
- Postprandial (after meal) Blood Sugar: Less than 140 mg/dL two hours after eating
- HbA1c (Average Blood Sugar over 2-3 months): Less than 5.7%
- Type 2 Diabetes: Prolonged hyperglycemia can lead to insulin resistance and ultimately, type 2 diabetes.
- Cardiovascular Disease: High blood sugar can damage blood vessels, increasing the risk of heart disease, stroke, and peripheral artery disease.
- Nerve Damage (Neuropathy): Elevated glucose levels can harm the nerves, causing pain, numbness, and tingling, particularly in the hands and feet.
- Kidney Damage (Nephropathy): High blood sugar can damage the small blood vessels in the kidneys, leading to kidney disease and eventual kidney failure.
- Eye Damage (Retinopathy): Hyperglycemia can damage the blood vessels in the retina, potentially leading to vision loss and blindness.
- Increased Risk of Infections: High blood sugar can weaken the immune system, making individuals more susceptible to infections.
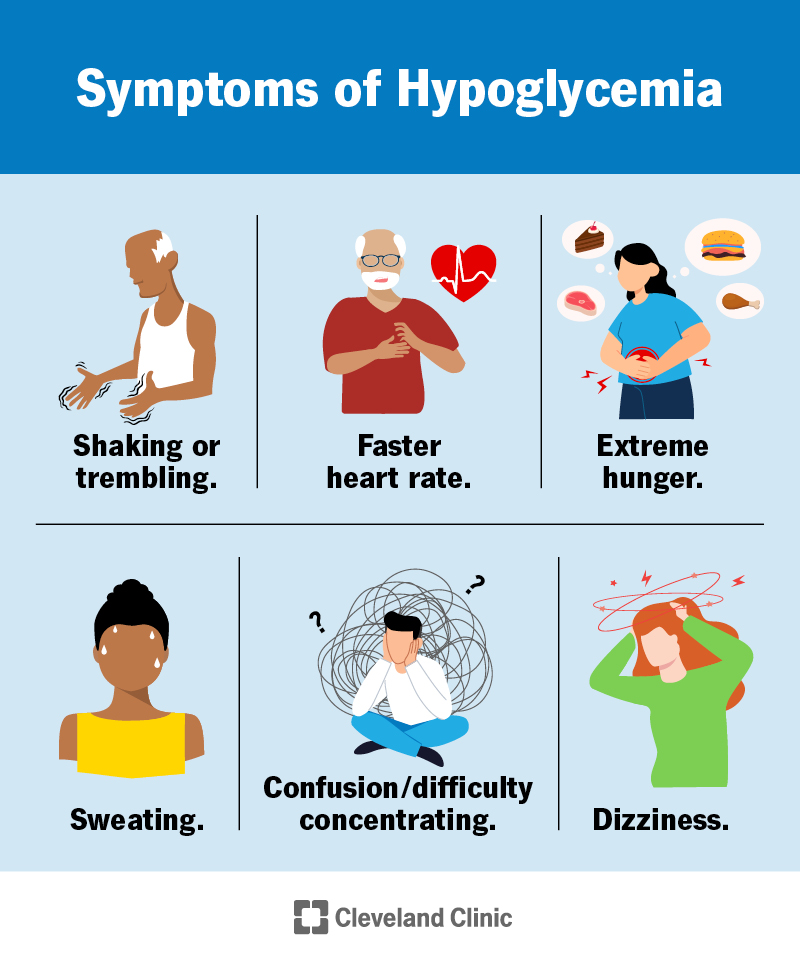
- Shakiness
- Sweating
- Dizziness
- Confusion
- Irritability
- Rapid Heartbeat
- Blurred Vision
- Loss of Consciousness
- Seizures
- Choose Low Glycemic Index (GI) Foods: The glycemic index measures how quickly a food raises blood sugar levels. Opt for foods with a low GI, such as whole grains, legumes, non-starchy vegetables, and fruits like berries and apples.
- Limit Processed Foods and Sugary Drinks: These foods are often high in refined carbohydrates and added sugars, which can cause rapid spikes in blood sugar.
- Focus on Fiber: Fiber slows down the absorption of glucose, helping to stabilize blood sugar levels. Include plenty of fiber-rich foods in your diet, such as vegetables, fruits, whole grains, and legumes.
- Balance Your Meals: Combine carbohydrates with protein and healthy fats to slow down glucose absorption and promote stable blood sugar levels.
- Portion Control: Be mindful of portion sizes to avoid overeating, which can lead to blood sugar spikes.
- Aerobic Exercise: Engage in activities like walking, jogging, swimming, or cycling for at least 30 minutes most days of the week.
- Strength Training: Incorporate strength training exercises to build muscle mass, which can further improve insulin sensitivity.
- Consistency is Key: Regular physical activity is more effective than sporadic bursts of exercise. Aim for a consistent exercise routine to reap the maximum benefits.
- Use a Blood Glucose Meter: Follow your healthcare provider’s recommendations for how often to check your blood sugar.
- Keep a Log: Record your blood sugar readings, along with information about your meals, exercise, and medications.
- Discuss Results with Your Healthcare Provider: Share your blood sugar logs with your healthcare provider to identify any trends or concerns and adjust your treatment plan as needed.
- Practice Relaxation Techniques: Engage in activities like meditation, yoga, deep breathing exercises, or spending time in nature to reduce stress.
- Get Enough Sleep: Aim for 7-8 hours of quality sleep each night. Sleep deprivation can increase stress hormones and impair insulin sensitivity.
- Seek Support: Talk to a therapist, counselor, or support group to manage stress and develop coping strategies.
- Follow Your Healthcare Provider’s Instructions: Take your medications as prescribed and understand their potential side effects.
- Monitor Blood Sugar Levels Regularly: Check your blood sugar levels regularly to assess the effectiveness of your medications.
- Communicate with Your Healthcare Provider: Report any concerns or side effects to your healthcare provider and work together to adjust your medication regimen as needed.
- Pack Snacks: Bring healthy snacks with you to prevent hypoglycemia, especially during long flights or car rides.
- Adjust Insulin Doses: If you’re traveling across time zones, work with your healthcare provider to adjust your insulin doses accordingly.
- Stay Hydrated: Drink plenty of water to prevent dehydration, which can affect blood sugar levels.
- Monitor Blood Sugar More Frequently: Check your blood sugar levels more often than usual to ensure they remain within a safe range.
- Continue Taking Your Medications: Even if you’re not eating as much, continue taking your diabetes medications as prescribed.
- Monitor Blood Sugar More Frequently: Check your blood sugar levels more often than usual to monitor the effects of illness.
- Stay Hydrated: Drink plenty of fluids to prevent dehydration.
- Contact Your Healthcare Provider: If you’re unable to keep food or fluids down, or if your blood sugar levels are consistently high or low, contact your healthcare provider.
- Check Blood Sugar Before, During, and After Exercise: Monitor your blood sugar levels to understand how your body responds to different types of exercise.
- Adjust Insulin Doses: If you take insulin, you may need to adjust your dosage before or after exercise to prevent hypoglycemia.
- Carry a Fast-Acting Carbohydrate Source: Keep glucose tablets or other fast-acting carbohydrates with you in case your blood sugar drops too low during exercise.
- Stay Hydrated: Drink plenty of water to prevent dehydration.
- Myth: Eating too much sugar causes diabetes.
- Fact: Type 2 diabetes is caused by a combination of genetic and lifestyle factors, including obesity, inactivity, and insulin resistance. While excessive sugar intake can contribute to weight gain and increase the risk of type 2 diabetes, it’s not the sole cause.
- Myth: People with diabetes can’t eat any sugar.
- Fact: People with diabetes can enjoy small amounts of sugar as part of a balanced diet. The key is to manage carbohydrate intake and monitor blood sugar levels.
- Myth: Diabetes is not a serious condition.
- Fact: Diabetes is a serious condition that can lead to numerous complications, including heart disease, kidney disease, nerve damage, and vision loss.
- Myth: Only overweight people get diabetes.
- Fact: While obesity is a major risk factor for type 2 diabetes, people of any weight can develop the condition. Genetics, ethnicity, and other lifestyle factors also play a role.
- Continuous Glucose Monitoring (CGM): CGMs provide real-time blood sugar readings and alerts, allowing for more proactive management.
- Insulin Pumps: Insulin pumps deliver a continuous dose of insulin, mimicking the body’s natural insulin release.
- Artificial Pancreas Systems: These systems combine a CGM and an insulin pump to automatically adjust insulin delivery based on blood sugar levels.
- New Medications: Researchers are developing new medications that can improve insulin sensitivity, lower blood sugar levels, and reduce the risk of complications.
- Link to another article on your site about “Low Glycemic Index Foods” when discussing dietary modifications. Anchor text: “Low Glycemic Index Foods”
- Link to an article about “Benefits of Regular Exercise” when discussing physical activity. Anchor text: “Benefits of Regular Exercise”
- Link to a page with information on “Continuous Glucose Monitoring” when discussing blood sugar monitoring. Anchor text: “Continuous Glucose Monitoring”
- Link to the American Diabetes Association (diabetes.org) for general information about diabetes. Link attribute: rel=”noopener”
- Link to the National Institute of Diabetes and Digestive and Kidney Diseases (niddk.nih.gov) for research and statistics on diabetes. Link attribute: rel=”noopener”
Key Takeaway: Knowing these ranges empowers you to monitor your blood sugar levels effectively and take appropriate action when necessary.
The Dangers of Unstable Blood Sugar
Unstable blood sugar levels, whether high or low, can pose significant health risks. Understanding these dangers is crucial for taking proactive steps to maintain balance. Let’s explore the potential consequences of both hyperglycemia and hypoglycemia.
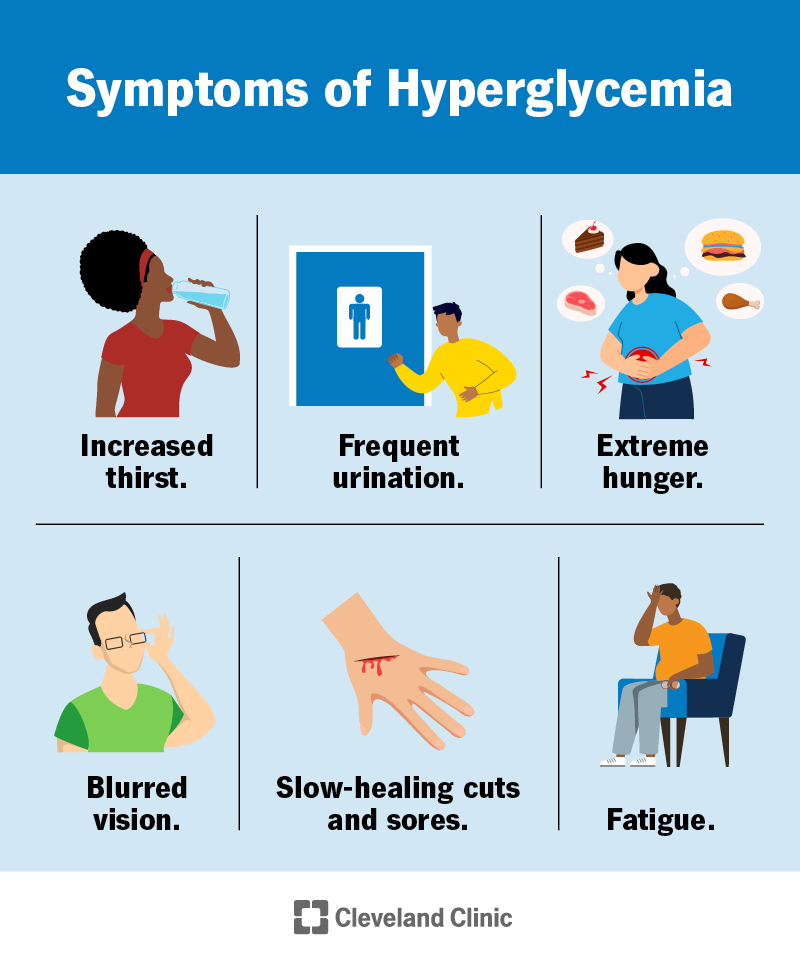
Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when there’s too much glucose in the blood. Over time, consistently high blood sugar levels can lead to serious complications, including:
Example: A person consistently consuming sugary drinks and processed foods may experience chronic hyperglycemia, significantly increasing their risk of developing type 2 diabetes and associated complications.
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop too low. This can happen for various reasons, including skipping meals, taking too much insulin, or engaging in intense physical activity without adequate carbohydrate intake. Symptoms of hypoglycemia can range from mild to severe and may include:
Important Note: Severe hypoglycemia can be life-threatening and requires immediate treatment.
Actionable Advice: If you experience symptoms of hypoglycemia, check your blood sugar levels immediately. If your blood sugar is below 70 mg/dL, consume a fast-acting source of carbohydrates, such as glucose tablets, fruit juice, or hard candy.
Strategies for Maintaining Blood Sugar Safety
Now that we understand the importance of blood sugar safety and the potential dangers of imbalance, let’s explore practical strategies to help you maintain healthy blood sugar levels.
Dietary Modifications
What you eat plays a significant role in regulating blood sugar. Making informed dietary choices can have a profound impact on your overall health.
Example: Instead of white bread, choose whole-grain bread. Instead of sugary soda, opt for water or unsweetened tea.
Regular Physical Activity
Exercise is a powerful tool for managing blood sugar. It helps improve insulin sensitivity, allowing your body to use glucose more effectively.
Practical Tip: Take a brisk walk after meals to help lower blood sugar levels.
Blood Sugar Monitoring
Regular blood sugar monitoring is essential, especially for individuals with diabetes. It allows you to track your blood sugar levels, identify patterns, and make informed decisions about your diet, exercise, and medication.
Recommendation: Consider using a continuous glucose monitor (CGM) for real-time blood sugar monitoring and alerts.
Stress Management
Stress can significantly impact blood sugar levels. When you’re stressed, your body releases hormones that can raise blood sugar.
Remember: Prioritizing stress management is crucial for maintaining stable blood sugar levels and overall well-being.
Medication Management
For individuals with diabetes, medication is often a necessary part of managing blood sugar.
Caution: Never adjust your medication dosage without consulting your healthcare provider.
Specific Situations and Blood Sugar Safety
Certain situations require extra attention to blood sugar safety. Understanding these scenarios can help you prepare and prevent potential complications.
Traveling
Traveling can disrupt your normal routine and make it challenging to manage blood sugar.
Tip: Carry a medical identification card or bracelet indicating that you have diabetes.
Illness
Illness can also affect blood sugar levels. When you’re sick, your body releases hormones that can raise blood sugar.
Important Note: Have a sick day plan in place with your healthcare provider.
Exercise
While exercise is beneficial for blood sugar management, it can also cause blood sugar levels to fluctuate.
Recommendation: Work with a certified diabetes educator or exercise physiologist to develop a safe and effective exercise plan.
Debunking Common Blood Sugar Myths
There are many misconceptions about blood sugar and diabetes. Let’s debunk some common myths to ensure you have accurate information.
Key Takeaway: Rely on credible sources and healthcare professionals for accurate information about blood sugar and diabetes.
The Future of Blood Sugar Management
Advancements in technology and research are continuously improving blood sugar management.
Exciting Development: The development of closed-loop systems, also known as artificial pancreases, promises to revolutionize diabetes management by automating insulin delivery and maintaining stable blood sugar levels.
Conclusion: Empowering Yourself for Blood Sugar Safety
Maintaining blood sugar safety is a lifelong journey that requires knowledge, awareness, and proactive management. By understanding the basics of blood sugar, recognizing the dangers of imbalance, and implementing practical strategies for maintaining healthy levels, you can empower yourself to thrive. Remember to prioritize a balanced diet, regular physical activity, stress management, and regular blood sugar monitoring. Stay informed, work closely with your healthcare provider, and embrace the advancements in technology that can help you achieve optimal blood sugar control. Your health is your wealth, and investing in blood sugar safety is an investment in a healthier, happier future.
Call to Action: Start today by making one small change to improve your blood sugar safety. Whether it’s choosing a healthier snack, taking a walk after dinner, or scheduling a check-up with your healthcare provider, every step counts.
Internal Linking Suggestions:
External Linking Suggestions:
Leave a Reply