Navigating Blood Sugar Safety: Your Comprehensive Guide to Staying Balanced and Healthy
Maintaining stable blood sugar levels is crucial for overall health and well-being. Whether you’re managing diabetes, pre-diabetes, or simply aiming for a healthier lifestyle, understanding blood sugar safety is essential. This guide will walk you through the ins and outs of blood sugar, offering practical tips, lifestyle adjustments, and strategies to keep your levels balanced and help you feel your best. Let’s dive in and explore how to navigate blood sugar safety together!

Understanding Blood Sugar: The Basics
Before we delve into safety measures, let’s establish a foundational understanding of what blood sugar is and why it matters.
What is Blood Sugar?
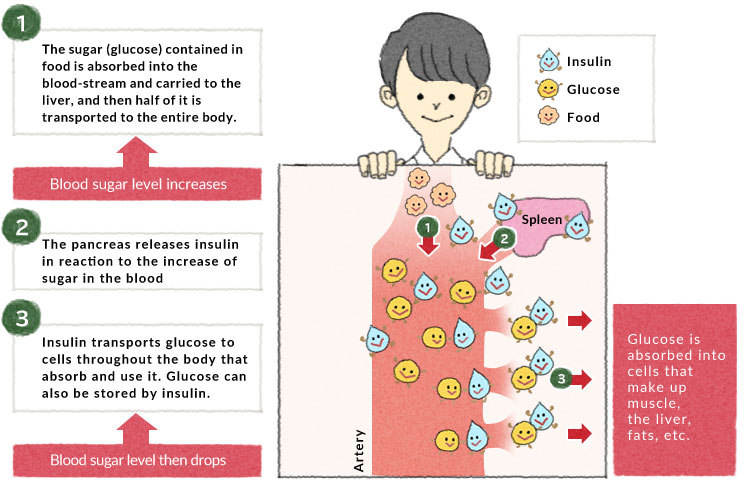
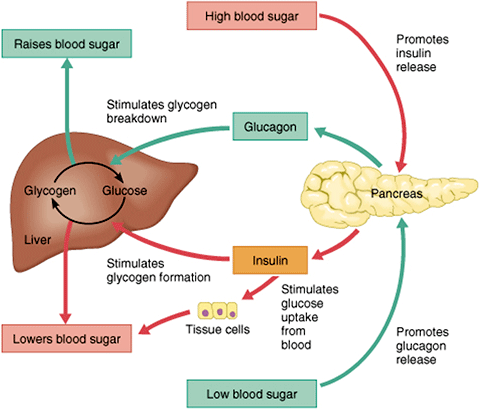
Blood sugar, or glucose, is the primary source of energy for your body. It comes from the food you eat, and your bloodstream carries it to cells throughout your body to provide fuel. Insulin, a hormone produced by the pancreas, helps glucose enter these cells.
Why is Blood Sugar Important?
Maintaining balanced blood sugar levels is vital for several reasons:
- Energy Levels: Stable blood sugar provides consistent energy, preventing energy crashes and fatigue.
- Organ Function: Proper blood sugar control supports the optimal function of vital organs like the brain, heart, and kidneys.
- Disease Prevention: Keeping blood sugar in a healthy range reduces the risk of developing type 2 diabetes, heart disease, and other chronic conditions.
- Fasting Blood Sugar: 70-100 mg/dL
- Postprandial (2 hours after eating): Less than 140 mg/dL
- HbA1c: Less than 5.7%
- Frequent urination
- Increased thirst
- Blurred vision
- Fatigue
- Slow-healing sores
- Diabetic Ketoacidosis (DKA): A life-threatening condition caused by a buildup of ketones in the blood.
- Hyperosmolar Hyperglycemic State (HHS): A severe condition characterized by extremely high blood sugar and dehydration.
- Long-Term Complications: Nerve damage (neuropathy), kidney damage (nephropathy), and eye damage (retinopathy).
- Shakiness
- Sweating
- Dizziness
- Confusion
- Irritability
- Rapid heartbeat
- Seizures: Severe hypoglycemia can lead to seizures and loss of consciousness.
- Brain Damage: Prolonged low blood sugar can deprive the brain of essential energy, leading to cognitive impairment.
- Coma: In extreme cases, hypoglycemia can result in a coma.
- Focus on Complex Carbohydrates: Choose whole grains, vegetables, and legumes over processed foods and sugary drinks. Complex carbs are digested slowly, providing a steady release of glucose into the bloodstream.
- Prioritize Fiber: High-fiber foods like fruits, vegetables, and whole grains help slow down glucose absorption, preventing rapid spikes in blood sugar.
- Include Lean Protein: Protein helps stabilize blood sugar levels and keeps you feeling full longer. Good sources include chicken, fish, beans, and tofu.
- Healthy Fats: Incorporate healthy fats like avocados, nuts, and olive oil into your diet. These fats can improve insulin sensitivity and support overall health.
- Limit Sugary Drinks and Processed Foods: Sugary drinks and processed foods can cause rapid spikes in blood sugar. Minimize your intake of these items to maintain stable levels.
- Regular Exercise: Physical activity helps improve insulin sensitivity and lowers blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Stress Management: Stress can raise blood sugar levels. Practice stress-reduction techniques like meditation, yoga, or deep breathing exercises.
- Adequate Sleep: Lack of sleep can disrupt hormone levels and affect blood sugar control. Aim for 7-9 hours of quality sleep each night.
- Hydration: Drink plenty of water throughout the day to help your kidneys flush out excess glucose.
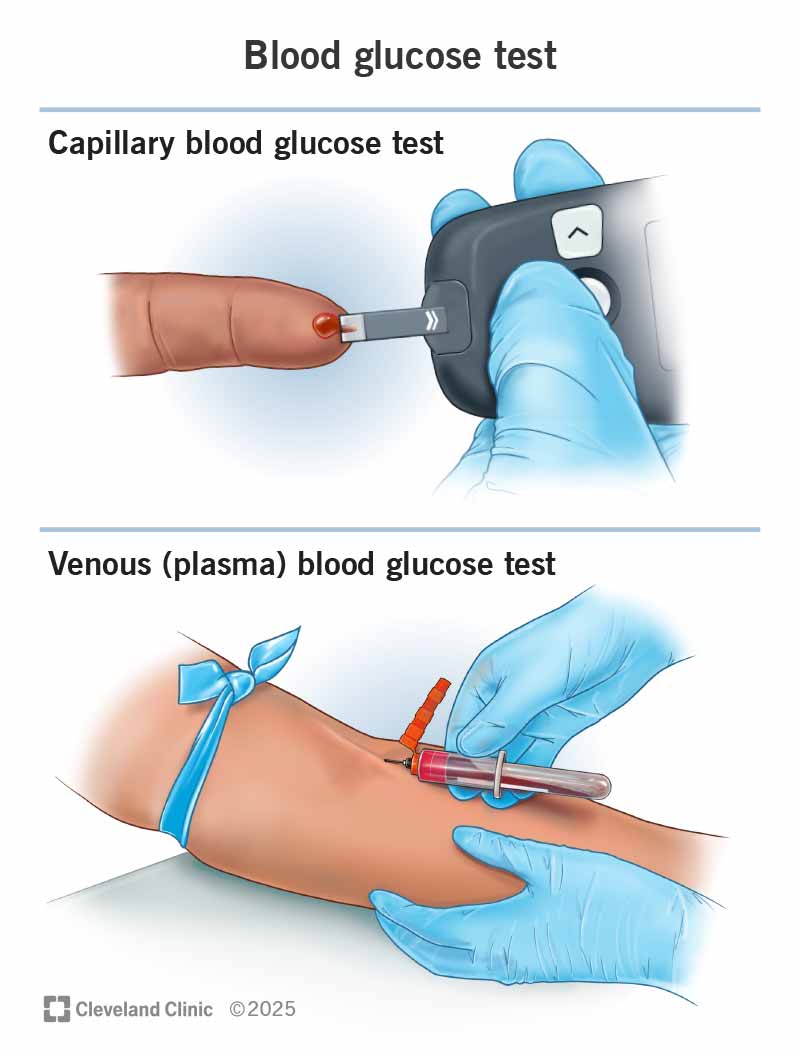
- Blood Glucose Meter: Use a blood glucose meter to check your blood sugar levels regularly. Follow your healthcare provider’s recommendations for testing frequency and timing.
- Continuous Glucose Monitoring (CGM): A CGM device tracks your blood sugar levels in real-time, providing valuable insights into trends and patterns.
- HbA1c Testing: This blood test provides an average of your blood sugar levels over the past 2-3 months. It’s a valuable tool for assessing long-term blood sugar control.
- Plan Ahead: Research local healthcare facilities and pharmacies in case you need medical assistance.
- Adjust Insulin: Consult with your healthcare provider about adjusting your insulin dosage based on time zone changes and activity levels.
- Carry Snacks: Keep a source of fast-acting carbohydrates on hand to prevent hypoglycemia.
- Adjust Insulin: If you take insulin, you may need to adjust your dosage before exercise to prevent low blood sugar.
- Monitor Blood Sugar: Check your blood sugar more frequently than usual.
- Adjust Medications: Consult with your healthcare provider about adjusting your medication dosages if you’re unable to eat or are experiencing vomiting or diarrhea.
- Make Healthy Choices: Choose lower-carb options and limit your intake of sugary drinks and desserts.
- Don’t Skip Meals: Skipping meals can lead to blood sugar imbalances.
- Myth: Eating too much sugar causes diabetes.
- Fact: Type 1 diabetes is an autoimmune condition, while type 2 diabetes is influenced by genetics, lifestyle factors, and insulin resistance.
- Myth: People with diabetes can’t eat any sugar.
- Fact: People with diabetes can enjoy small amounts of sugar as part of a balanced meal plan.
- Myth: Diabetes is not a serious condition.
- Fact: Diabetes can lead to serious complications if not managed properly.
- Myth: Only overweight people develop type 2 diabetes.
- Fact: While obesity is a risk factor, people of all sizes can develop type 2 diabetes.
- Continuous Glucose Monitors (CGMs): CGMs provide real-time blood sugar readings and alerts, helping you stay ahead of potential highs and lows.
- Insulin Pumps: Insulin pumps deliver a steady stream of insulin throughout the day, mimicking the way a healthy pancreas works.
- Smart Insulin Pens: These pens track insulin dosages and provide reminders, helping you stay on track with your medication.
- Mobile Apps: Numerous mobile apps are available to help you track your blood sugar, diet, exercise, and medications.
- Artificial Pancreas Systems: These systems automatically adjust insulin delivery based on real-time blood sugar readings, providing a closed-loop system for blood sugar control.
- A: If your blood sugar is high, drink plenty of water, avoid sugary drinks, and follow your healthcare provider’s recommendations for adjusting your medication.
- A: If your blood sugar is low, consume 15 grams of carbohydrates, wait 15 minutes, and then recheck your blood sugar. Repeat if necessary.
- A: The frequency of blood sugar monitoring depends on your individual needs and treatment plan. Follow your healthcare provider’s recommendations.
- A: Yes, stress can raise blood sugar levels. Practice stress-reduction techniques to help manage your blood sugar.
- A: Focus on complex carbohydrates, fiber-rich foods, lean protein, and healthy fats.
- A: Yes, exercise is safe and beneficial for people with diabetes. However, it’s important to monitor your blood sugar and adjust your medication as needed.

Normal Blood Sugar Ranges
Understanding normal blood sugar ranges is the first step in ensuring your safety. Here’s a general guideline:
Note: These ranges can vary depending on individual health conditions and should be discussed with your healthcare provider.

Recognizing the Dangers: High and Low Blood Sugar
Both high and low blood sugar levels can pose significant health risks. Recognizing the symptoms and understanding the potential dangers is crucial for taking timely action.
Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when there’s too much glucose in the blood. This can happen if your body doesn’t produce enough insulin or if your cells become resistant to insulin.
Symptoms of Hyperglycemia:
Dangers of Hyperglycemia:
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop too low. This can happen if you take too much insulin, skip meals, or engage in intense physical activity without adjusting your medication or food intake.
Symptoms of Hypoglycemia:
Dangers of Hypoglycemia:
Key Takeaway: Recognizing the symptoms of both high and low blood sugar is crucial for timely intervention and preventing serious health complications. Always consult with your healthcare provider for personalized advice and treatment.
Practical Tips for Maintaining Blood Sugar Safety
Now that we understand the basics and the potential dangers, let’s explore practical tips for maintaining blood sugar safety. These strategies encompass dietary adjustments, lifestyle changes, and monitoring techniques.
Dietary Strategies
What you eat plays a significant role in regulating blood sugar levels. Here are some dietary strategies to consider:
Lifestyle Adjustments
In addition to dietary changes, certain lifestyle adjustments can significantly impact blood sugar control.
Monitoring Techniques
Regular monitoring is essential for understanding how your body responds to different foods, activities, and medications.
Internal Link Suggestion: For more information on continuous glucose monitoring, link to a relevant article on your website using the anchor text “CGM devices.”
Creating a Blood Sugar Safety Plan
A well-thought-out blood sugar safety plan is crucial for managing your health effectively. Here’s how to create one:
Step 1: Consult with Your Healthcare Provider
Work closely with your doctor, diabetes educator, and registered dietitian to develop a personalized plan that meets your specific needs.
Step 2: Set Realistic Goals
Establish achievable goals for blood sugar levels, diet, exercise, and other lifestyle factors.
Step 3: Develop a Meal Plan
Create a detailed meal plan that includes balanced meals and snacks. Consider working with a registered dietitian to ensure your plan is nutritionally sound and tailored to your needs.
Step 4: Establish an Exercise Routine
Design an exercise routine that you enjoy and can stick with long-term. Incorporate both aerobic and strength-training exercises for optimal benefits.
Step 5: Learn How to Manage Stress
Identify your stress triggers and develop coping strategies. Techniques like mindfulness, yoga, and spending time in nature can be helpful.
Step 6: Monitor Your Blood Sugar Regularly
Keep a log of your blood sugar readings and note any patterns or trends. Share this information with your healthcare provider to make informed decisions about your treatment plan.
Step 7: Know How to Treat Hypoglycemia
Always carry a fast-acting source of glucose, such as glucose tablets or juice, in case your blood sugar drops too low. Follow the “15-15 rule”: Consume 15 grams of carbohydrates, wait 15 minutes, and then recheck your blood sugar.
Step 8: Understand When to Seek Medical Attention
Know the signs and symptoms of serious blood sugar imbalances and when to seek immediate medical attention.
Example: John, a 55-year-old with type 2 diabetes, worked with his healthcare team to create a blood sugar safety plan. He set a goal to walk for 30 minutes each day, follow a low-carb meal plan, and monitor his blood sugar levels twice daily. By adhering to his plan, John successfully lowered his HbA1c from 7.5% to 6.2% and improved his overall health.
Blood Sugar Safety in Specific Situations
Blood sugar management can be particularly challenging in certain situations. Here’s how to navigate some common scenarios:
Traveling
* Pack Smart: Carry all your medications, testing supplies, and snacks in your carry-on luggage.
Exercise
* Check Blood Sugar: Monitor your blood sugar before, during, and after exercise.
Illness
* Stay Hydrated: Drink plenty of fluids to prevent dehydration.
Special Occasions
* Plan Ahead: If you’re attending a party or holiday gathering, plan your meals and snacks in advance.
External Link Suggestion: Link to the American Diabetes Association’s website using the anchor text “diabetes resources” for additional information on managing diabetes in various situations.
Debunking Common Myths About Blood Sugar
There are many misconceptions about blood sugar and diabetes. Let’s debunk some common myths:
Key Takeaway: Staying informed and relying on credible sources can help you make informed decisions about your health and well-being.
The Role of Technology in Blood Sugar Safety
Technology has revolutionized the way we manage blood sugar. Here are some technological advancements that can enhance blood sugar safety:
Internal Link Suggestion: Link to a blog post discussing the latest advancements in diabetes technology using the anchor text “diabetes technology.”
Frequently Asked Questions (FAQ) About Blood Sugar Safety
Here are some frequently asked questions about blood sugar safety:
Q: What should I do if my blood sugar is too high?
Q: What should I do if my blood sugar is too low?
Q: How often should I check my blood sugar?
Q: Can stress affect my blood sugar?
Q: What are the best foods for maintaining stable blood sugar?
Q: Is exercise safe if I have diabetes?
Conclusion: Empowering You to Take Control of Your Blood Sugar
Navigating blood sugar safety is a journey that requires knowledge, commitment, and a proactive approach. By understanding the basics of blood sugar, recognizing the dangers of imbalances, and implementing practical strategies, you can take control of your health and well-being. Remember to consult with your healthcare provider to develop a personalized plan that meets your specific needs, and stay informed about the latest advancements in blood sugar management. Embrace a balanced lifestyle, prioritize self-care, and empower yourself to live a healthy and fulfilling life with stable blood sugar levels.
Call to Action: Ready to take control of your blood sugar safety? Sign up for our newsletter to receive regular tips, updates, and exclusive content on managing your health effectively!
Leave a Reply