Navigating Blood Sugar Safety: A Comprehensive Guide to Staying Balanced and Healthy
Maintaining stable blood sugar levels is crucial for overall health and well-being. Think of your blood sugar as the fuel gauge for your body – too high or too low, and things just won’t run smoothly. This comprehensive guide will walk you through everything you need to know about blood sugar safety, from understanding the basics to implementing practical strategies for keeping your levels in a healthy range. We’ll cover the importance of blood sugar, common conditions related to imbalances, practical tips for managing your levels, and when to seek professional help. So, let’s dive in and empower you to take control of your blood sugar and your health!

Understanding Blood Sugar Basics
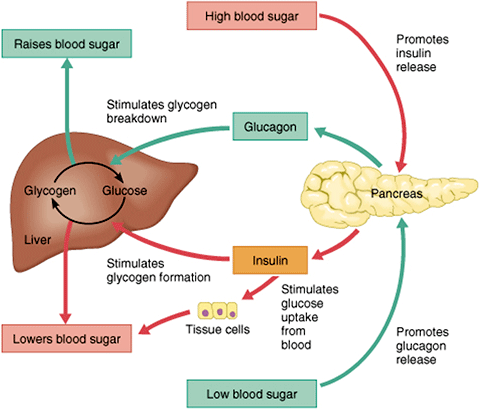
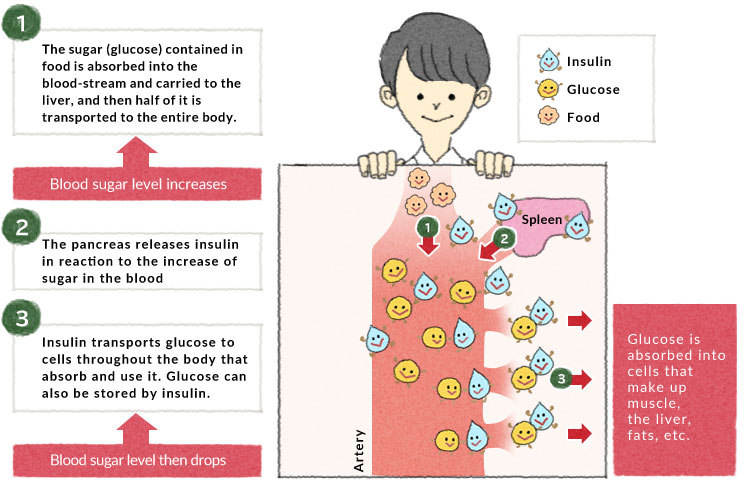
Before we delve into safety, let’s establish a solid understanding of what blood sugar actually is. Blood sugar, or glucose, is the primary source of energy for your body. It comes from the food you eat, particularly carbohydrates. After you eat, your digestive system breaks down carbohydrates into glucose, which then enters your bloodstream.
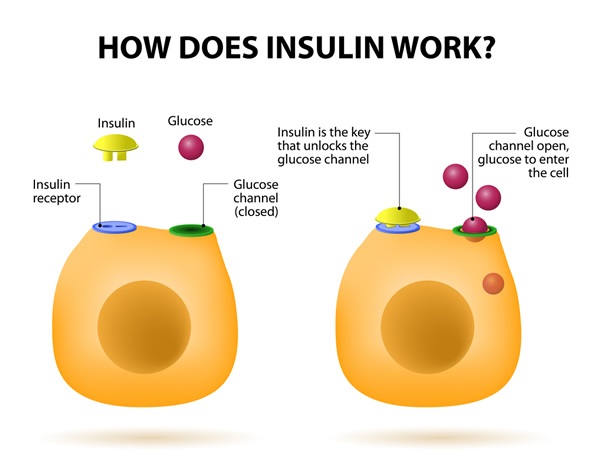
The Role of Insulin
Now, here’s where insulin comes into play. Insulin is a hormone produced by your pancreas. Its main job is to act like a key, unlocking your cells to allow glucose to enter and be used for energy. Without insulin, glucose would just float around in your bloodstream, unable to fuel your cells.

Normal Blood Sugar Ranges
Maintaining blood sugar within a normal range is essential for optimal health. Generally, normal blood sugar levels are:
- Fasting (before eating): 70-100 mg/dL
- 2 hours after eating: Less than 140 mg/dL
- Diabetes (Type 1 and Type 2)
- Overeating
- Lack of physical activity
- Illness or infection
- Certain medications
- Increased thirst
- Frequent urination
- Blurred vision
- Fatigue
- Slow-healing sores
- Headaches
- Heart disease
- Kidney disease
- Nerve damage (neuropathy)
- Eye damage (retinopathy)
- Increased risk of infections
- Excessive insulin dosage
- Skipping or delaying meals
- Intense exercise
- Alcohol consumption (especially on an empty stomach)
- Certain medications
- Shakiness
- Sweating
- Dizziness
- Confusion
- Irritability
- Rapid heartbeat
- Hunger
- Blurred vision
- Seizures (in severe cases)
- Loss of consciousness (in severe cases)
- Check your blood sugar: If it’s below 70 mg/dL, proceed to step 2.
- Consume 15 grams of fast-acting carbohydrates: Examples include glucose tablets, fruit juice, regular soda (not diet), or hard candies.
- Wait 15 minutes: Recheck your blood sugar.
- Repeat if necessary: If your blood sugar is still below 70 mg/dL, repeat steps 2 and 3.
- Eat a meal or snack: Once your blood sugar is above 70 mg/dL, eat a meal or snack to stabilize your levels and prevent another drop.
- Family history of diabetes
- Overweight or obesity
- Physical inactivity
- Age 45 or older
- High blood pressure
- Abnormal cholesterol levels
- Gestational diabetes (diabetes during pregnancy)
- High blood pressure
- Preeclampsia
- Large birth weight (macrosomia)
- Increased risk of cesarean delivery
- Increased risk of developing type 2 diabetes later in life for the mother
- Increased risk of obesity and type 2 diabetes for the child later in life
- Dietary changes
- Regular exercise
- Blood sugar monitoring
- In some cases, insulin therapy
- Whole Grains: Choose whole grains like brown rice, quinoa, and whole-wheat bread over refined grains like white bread and white rice. Whole grains are digested more slowly, leading to a more gradual rise in blood sugar.
- Lean Proteins: Include lean protein sources like chicken, fish, beans, and lentils in your meals. Protein helps stabilize blood sugar levels and keeps you feeling full.
- Healthy Fats: Incorporate healthy fats like avocados, nuts, seeds, and olive oil into your diet. These fats can improve insulin sensitivity and help regulate blood sugar.
- Fruits and Vegetables: Load up on a variety of colorful fruits and vegetables. They’re packed with fiber, vitamins, and minerals, and have a lower impact on blood sugar than processed foods. Be mindful of portion sizes with fruits, as they do contain natural sugars.
- Limit Sugary Drinks and Processed Foods: Avoid sugary drinks like soda, juice, and sweetened tea, as they can cause rapid spikes in blood sugar. Also, limit your intake of processed foods, which are often high in unhealthy fats, sugar, and sodium.
- Breakfast: Oatmeal with berries and nuts, a side of Greek yogurt
- Lunch: Salad with grilled chicken or chickpeas, avocado, and a vinaigrette dressing
- Dinner: Baked salmon with roasted vegetables (broccoli, carrots, and sweet potatoes)
- Snacks: Apple slices with almond butter, a handful of almonds, or a small serving of Greek yogurt
- Aim for at least 150 minutes of moderate-intensity exercise per week: This could include brisk walking, cycling, swimming, or dancing.
- Incorporate strength training exercises at least twice a week: Strength training helps build muscle mass, which can improve insulin sensitivity and help regulate blood sugar.
- Find activities you enjoy: The key to sticking with an exercise routine is to find activities you genuinely enjoy. Whether it’s hiking, yoga, or playing a sport, choose activities that you look forward to.
- Monitor your blood sugar before, during, and after exercise: This will help you understand how exercise affects your blood sugar levels and adjust your food intake or insulin dosage accordingly.
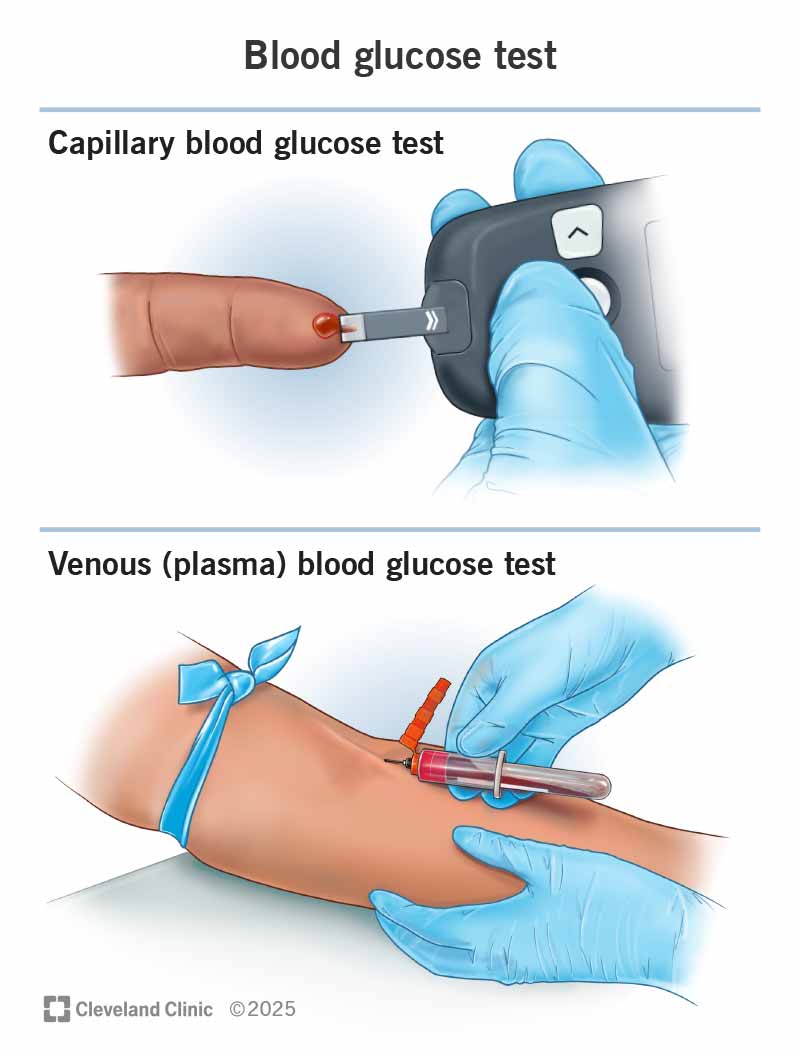
- Use a blood glucose meter: A blood glucose meter is a small device that measures the amount of glucose in your blood. You’ll need to prick your finger with a lancet to obtain a small blood sample, which you then apply to a test strip that is inserted into the meter.
- Follow your healthcare provider’s recommendations for testing frequency: The frequency of blood sugar monitoring will vary depending on your individual needs and treatment plan. Some people may need to check their blood sugar several times a day, while others may only need to check it once a day or less.
- Keep a log of your blood sugar readings: This will help you track your progress and identify patterns or trends. Share your log with your healthcare provider so they can make adjustments to your treatment plan as needed.
- Consider Continuous Glucose Monitoring (CGM): A CGM is a device that continuously monitors your blood sugar levels throughout the day and night. It consists of a small sensor that is inserted under your skin and transmits data to a receiver or smartphone. CGMs can provide valuable insights into how your blood sugar levels fluctuate in response to different factors, such as food, exercise, and stress.
- Practice relaxation techniques: Techniques like deep breathing, meditation, and yoga can help reduce stress and lower blood sugar levels.
- Get enough sleep: Aim for 7-8 hours of sleep per night. Lack of sleep can increase stress hormones and negatively affect blood sugar control.
- Engage in enjoyable activities: Make time for hobbies and activities that you find relaxing and enjoyable. This could include reading, listening to music, spending time in nature, or pursuing a creative outlet.
- Seek support: Talk to a therapist, counselor, or support group if you’re struggling to manage stress.
- Aim for at least 8 glasses of water per day: Water helps flush out excess glucose from the body and keeps you feeling hydrated.
- Avoid sugary drinks: As mentioned earlier, sugary drinks can cause rapid spikes in blood sugar. Stick to water, unsweetened tea, or other low-calorie beverages.
- Drink alcohol in moderation: If you choose to drink alcohol, do so in moderation. This means no more than one drink per day for women and no more than two drinks per day for men.
- Eat food when drinking alcohol: Eating food while drinking alcohol can help slow down the absorption of alcohol and prevent blood sugar from dropping too low.
- Monitor your blood sugar levels: Check your blood sugar levels before, during, and after drinking alcohol to see how it affects you.
- Talk to your healthcare provider about any medications you’re taking: This includes prescription medications, over-the-counter medications, and supplements.
- Be aware of the potential side effects of your medications: Some medications, such as steroids and certain antidepressants, can raise blood sugar levels.
- Follow your healthcare provider’s instructions carefully: Take your medications as prescribed and don’t change the dosage without talking to your healthcare provider first.
- Pack your medications and supplies: Make sure you have enough medication and supplies to last for the entire trip.
- Bring snacks: Pack healthy snacks to prevent low blood sugar.
- Stay active: Try to maintain your exercise routine as much as possible.
- Monitor your blood sugar levels more frequently: Check your blood sugar levels more often than usual to see how travel affects you.
- If you experience frequent or severe episodes of hypoglycemia or hyperglycemia: This could indicate that your treatment plan needs adjustment.
- If you have symptoms of diabetes: Increased thirst, frequent urination, unexplained weight loss, and fatigue are all potential signs of diabetes.
- If you have risk factors for diabetes: Family history, obesity, and physical inactivity increase your risk of developing diabetes.
- If you’re pregnant or planning to become pregnant: Gestational diabetes requires specialized care.
- If you have any concerns about your blood sugar levels or your overall health: Don’t hesitate to reach out to your healthcare provider for guidance.
- Anchor Text: “Symptoms of Hyperglycemia” -> Link to the section discussing hyperglycemia symptoms.
- Anchor Text: “15-15 rule” -> Link to the section explaining the 15-15 rule for hypoglycemia.
- Anchor Text: “Continuous Glucose Monitoring (CGM)” -> Link to the section explaining CGM.
- Anchor Text: “healthy diet” -> Link to the section on embracing a balanced diet.
- Anchor Text: “regular exercise” -> Link to the section on getting moving with regular exercise.
- American Diabetes Association (ADA): Link to the ADA website for comprehensive information on diabetes. Use anchor text like “American Diabetes Association” or “diabetes resources.” Attribute link with “rel=noopener” to ensure security.
https://www.diabetes.org/- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Link to the NIDDK website for research and information on diabetes and related conditions. Use anchor text like “NIDDK” or “diabetes research.” Attribute link with “rel=noopener” to ensure security.
https://www.niddk.nih.gov/- Centers for Disease Control and Prevention (CDC): Link to the CDC website for information on diabetes prevention and management. Use anchor text like “CDC diabetes information” or “diabetes prevention.” Attribute link with “rel=noopener” to ensure security.
https://www.cdc.gov/diabetes/index.html
These ranges can vary slightly depending on individual factors and testing methods, so it’s always best to consult with your healthcare provider for personalized guidance.

Why Blood Sugar Matters
Why all the fuss about keeping blood sugar levels in check? Well, consistently high or low blood sugar can lead to a host of health problems. Think of it like this: constantly revving your car engine too high or letting it run on empty – it’s not sustainable and will eventually cause damage.

Common Conditions Related to Blood Sugar Imbalances
When blood sugar levels are consistently outside the normal range, it can lead to several health conditions. Let’s explore some of the most common ones:
Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when there’s too much glucose in the blood. This can happen if your body doesn’t produce enough insulin, or if your cells become resistant to insulin’s effects. Common causes include:
Symptoms of Hyperglycemia:
Long-Term Risks:
If left unmanaged, chronic hyperglycemia can lead to serious complications, including:
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop too low. This can happen if you take too much insulin, skip meals, or exercise intensely without enough fuel.
Common Causes:
Symptoms of Hypoglycemia:
Immediate Action:
Hypoglycemia requires immediate action. The “15-15 rule” is a helpful guideline:
When to Seek Emergency Help:
If someone with hypoglycemia becomes unconscious or has a seizure, it’s crucial to seek immediate medical attention. Glucagon, a hormone that raises blood sugar levels, can be administered in these situations.
Prediabetes
Prediabetes is a condition where blood sugar levels are higher than normal but not high enough to be diagnosed as type 2 diabetes. It’s often considered a warning sign that diabetes may develop in the future.
Risk Factors:
Importance of Early Detection:
The good news is that prediabetes is often reversible with lifestyle changes. Losing weight, eating a healthy diet, and getting regular exercise can help lower blood sugar levels and prevent the progression to type 2 diabetes.
Gestational Diabetes
Gestational diabetes develops during pregnancy in women who didn’t have diabetes before. It’s caused by hormonal changes that make it harder for the body to use insulin effectively.
Risks to Mother and Baby:
Gestational diabetes can increase the risk of complications during pregnancy and delivery, including:
Management:
Managing gestational diabetes typically involves:
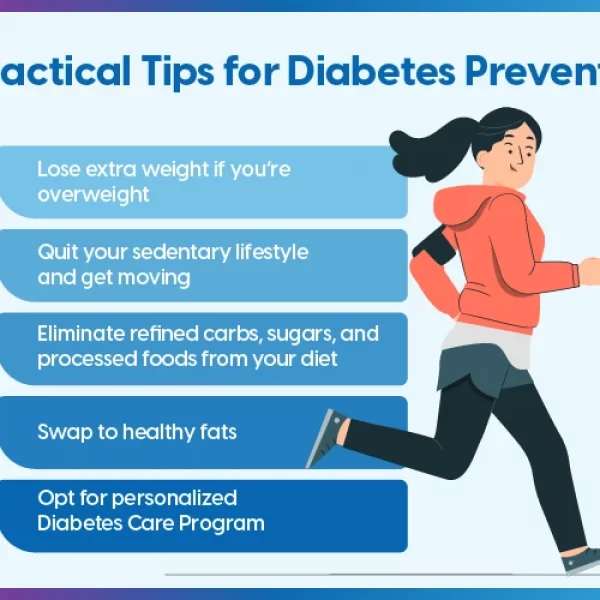
Practical Tips for Managing Blood Sugar Levels
Now that we’ve covered the basics and common conditions, let’s move on to practical strategies for managing your blood sugar levels and staying safe.
1. Embrace a Balanced Diet
A healthy diet is the cornerstone of blood sugar management. Focus on:
Example Meal Plan:
2. Get Moving with Regular Exercise
Physical activity is a powerful tool for managing blood sugar. Exercise helps improve insulin sensitivity, meaning your body can use insulin more effectively to transport glucose into your cells.
3. Monitor Your Blood Sugar Regularly
Regular blood sugar monitoring is essential for understanding how your body responds to food, exercise, and medication.
4. Manage Stress Effectively
Stress can have a significant impact on blood sugar levels. When you’re stressed, your body releases hormones like cortisol and adrenaline, which can raise blood sugar.
5. Stay Hydrated
Drinking enough water is crucial for overall health and can also help regulate blood sugar levels.
6. Monitor Alcohol Consumption
Alcohol can affect blood sugar levels in unpredictable ways. It can initially cause blood sugar to rise, but then lead to a drop in blood sugar later on.
7. Be Mindful of Medications
Certain medications can affect blood sugar levels.
8. Plan Ahead for Travel
Traveling can disrupt your routine and make it challenging to manage your blood sugar.
When to Seek Professional Help
While many aspects of blood sugar management can be handled through lifestyle adjustments, there are times when professional medical advice is essential.
Internal Linking Opportunities
To further enhance user experience and SEO, here are some internal linking opportunities:
External Linking Opportunities
To provide additional resources and credibility, here are some external linking opportunities:
Conclusion: Empowering You to Take Control
Managing your blood sugar levels is a lifelong journey, but it’s one that’s well worth the effort. By understanding the basics of blood sugar, recognizing the signs of imbalances, and implementing practical strategies for staying balanced, you can empower yourself to take control of your health and well-being. Remember, small changes can make a big difference. Start with one or two of the tips we’ve discussed today and gradually incorporate more as you become comfortable. And don’t hesitate to reach out to your healthcare provider for personalized guidance and support. Your health is your greatest asset – invest in it wisely!